
IBD and Pregnancy: The Good News
Are you at a point in your life where you’re thinking about starting a family? Maybe you and your partner have been considering it for a while now, wondering what it’s like to have a little one running around the house, and have been sharing cute baby photos and making wishlists filled with cribs and toys. This is a fun time! However, if you have inflammatory bowel disease (IBD), you might have some concerns about how the disease, along with its treatments, might affect your pregnancy. The good news is that most women with IBD have normal, healthy pregnancies.
Fertility and Genetic Risk
If you’re a woman and your Crohn’s disease or ulcerative colitis (the two main types of IBD) is under control and you have not undergone surgery for IBD, then you have similar fertility rates to the general public.1 Age continues to be the biggest risk factor for decreased fertility whether you live with IBD or not. However, active inflammation, surgeries such as a j-pouch or proctectomy, or having a permanent ostomy, could affect your fertility.1,2
For men with IBD, disease activity, medications, poor lifestyle and dietary habits (such as alcohol and tobacco use and an unhealthy diet), and rectal surgery may affect your fertility.3
Depending on your age, type of IBD, and treatment history, you might want to speak with your doctor before starting a family to find out what you need to know so you can have a healthy pregnancy. You should also ask them early on about family planning and preconception counselling.
When you’re diagnosed with IBD, it might run through your head that you could pass this on to your children. The good news is that if you or your partner have IBD, the genetic risk of disease transmission to your child is only 2-3%. However, if both partners have IBD, the risk increases to more than 30%,1 so your family doctor might refer you for genetic counselling.
Medications
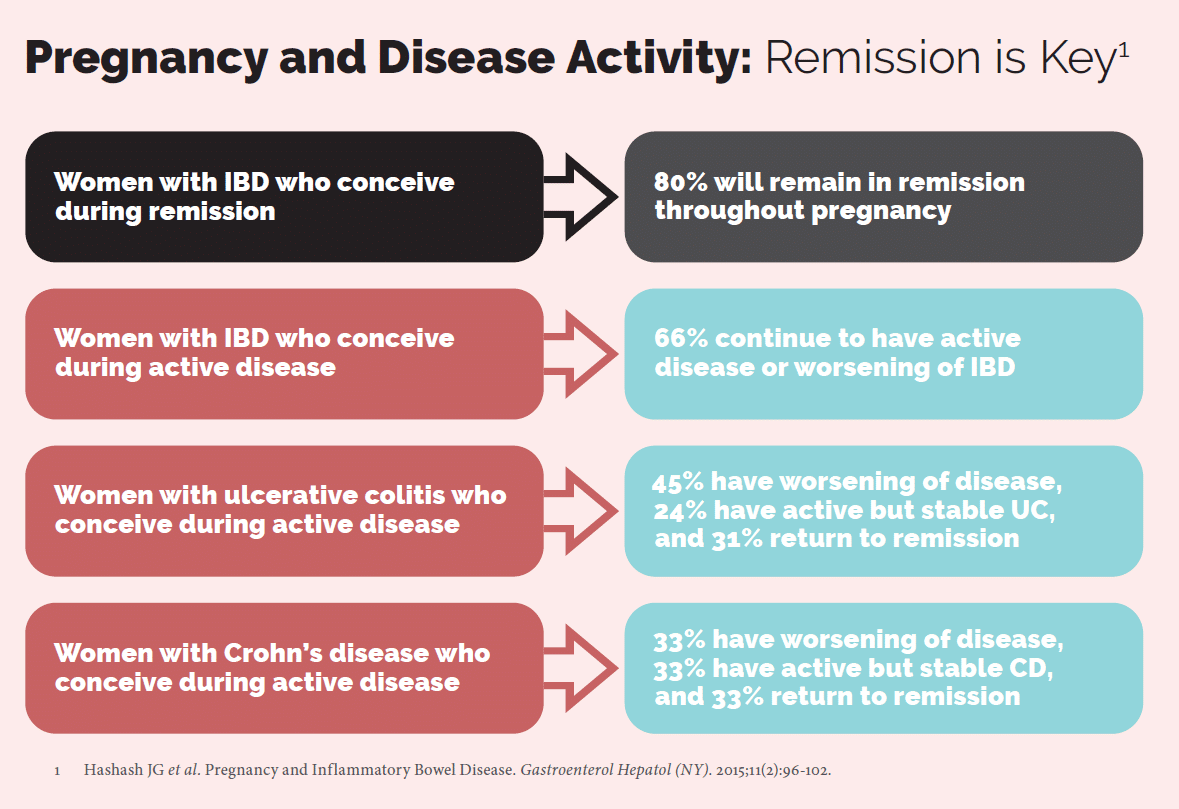
Remission is crucial to ensure a safe pregnancy. Studies show that 80% of women in remission will maintain disease inactivity throughout pregnancy.4 However, doctors do not recommend becoming pregnant if your IBD is active, since this may lead to increased risks of adverse outcomes, including disease worsening and delivery complications.
Studies have also found that a majority of IBD medications are safe to use during pregnancy and have low transmission to breastmilk. 1,2 Consult your doctor to learn more, especially since your dosing regimen may change during conception and throughout your pregnancy.
Regarding long-term health outcomes, a population-based study in Denmark5 shows that children exposed to azathioprine and mercaptopurine in utero do not develop an increased risk for infections in their childhood, adolescence, and adulthood. However, children exposed to anti-TNF biologics develop an increased risk of infections in their first year of life. With both types of medications, there were no increased risks for autism spectrum disorder, attention deficit hyperactivity disorder, psychiatric illnesses, or cancers in major organs.
The IBD in Pregnancy Consensus Group recommends that biologic therapies should resume immediately after giving birth and under the same dosing regimen to prevent the risk of flares and disease activity.6
We strongly recommend that you do not discontinue your medications without consulting your gastroenterologist, since doing so can trigger a flare and may lead to adverse outcomes to your health and your child.
Delivery
In most cases, women will have the option to give birth via standard vaginal delivery.1 If you have had ileal pouch-anal anastomosis surgery, your obstetrician-gynecologist might recommend a Cesarian section (C-section) to prevent anal sphincter injury. They may also suggest a C-section if you have perianal disease, active IBD, or a prior Cesarian delivery. Choosing the best mode of delivery will require collaborative decision-making between you and your healthcare team.
Vaccines
Except for certolizumab (Cimzia®), research shows that biologic therapies transfer to infants if you are receiving it during pregnancy.2 It can take up to 12 months for the antibodies to disappear. After this period, your baby can safely receive live vaccines. Consult your child’s pediatrician on their recommendations for scheduling vaccines.
Discontinuing biologic medication before the third trimester might increase your risk of disease relapse and infections in your child so it’s important that you adhere to your medications and consult your healthcare team with any concerns throughout your pregnancy.
Outlook
With the support of a multidisciplinary healthcare team and education, you can be confident about your medication choices and have a safe pregnancy while keeping your inflammatory bowel disease under control. Soon you’ll be sharing pictures of your own bundle of joy!















