Breaking the Link – IBS and Bacterial Overgrowth
Attributing irritable bowel syndrome (IBS) to bacterial overgrowth may be a mistake. According to Swedish researchers in a 2007 report published in the medical journal, Gut, the misguided assumption could be due to ineffective testing methods used in previous studies.
IBS is a common digestive disorder characterized by abdominal pain, bloating, constipation, and/or diarrhea, affecting up to 20% of the Canadian population.
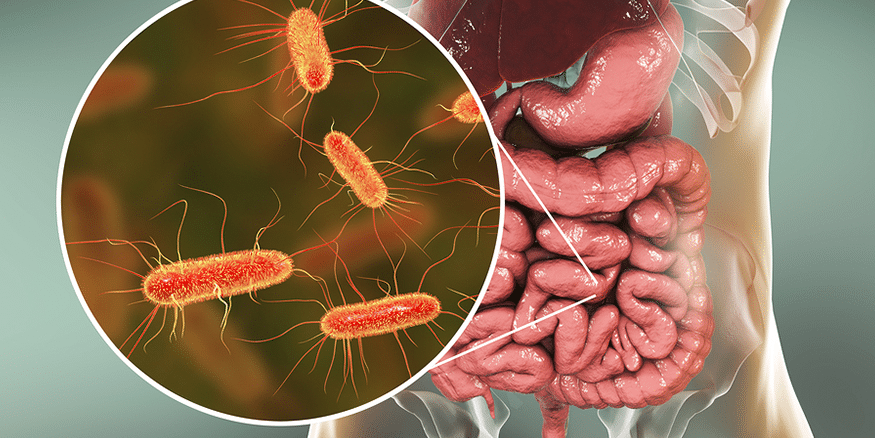
One theory is that IBS results from an increased number of unfriendly bacteria in the small intestine. This condition is called small intestinal bacterial overgrowth, or SIBO, which we first reported in The Inside Tract®, issue 129 (January/February 2002). SIBO is thought to arise when naturally occurring bacteria from the colon over-populate in the small intestine, or when the gastric-acid barrier fails.
Various bacteria found in the gut include Escherichia coli, Staphylococcus aureus, Clorstridium, Enterobacter, Klebsiella, and mixed G-flora. Normally, the upper portion of the small bowel contains Gram-positive bacteria. Gram-negative bacteria are low in number and anaerobes are rare, therefore, growth of these bacteria in an area where they don’t naturally belong represents SIBO. Bacteria multiply in greater numbers progressively along the digestive tract. To illustrate, here are some sampled bacteria quantities: (measured in colony forming units/millilitre, or cfu/ml)
| Duodenum & jejunum | 100-4 |
| Proximal ileum | 100-5 |
| Terminal ileum | 105-8 |
| Cecum | 1010-12 |
According to the Swedish researchers, the evidence for true cases of SIBO is in the testing methods. Previous researchers looking into SIBO tested bacterial levels indirectly, used the lactulose hydrogen breath test (LHBT), which measures exhaled concentrations of the gases hydrogen and methane produced by intestinal bacteria. This test is not considered to be as accurate or reliable as the glucose hydrogen breath test (GHBT) or the C-xylose test.
In this study, researchers drew samples from the jejunal contents (the middle portion of the small intestine) and then cultured them for a more direct indication of bacterial levels. Many consider this direct testing to be the gold standard to determine whether a patient has SIBO.
For comparison purposes, the researchers also tested patients with and without IBS using the LHBT and the more effective GHBT. They then evaluated these results, alongside results from the direct testing of bacterial cultures. When tested with the LHBT, patients were more likely to show a positive result for SIBO, which did not hold true when compared with a direct colonic culture.
86% of those who tested positive with the LHBT also showed abnormal intestinal movement, compared with only 39% of the patients without SIBO. However, while prior evidence indicated antibiotic treatment to be moderately effective in treating irritable bowel syndrome patients who were diagnosed with SIBO using the LHTB, the current study showed no improvement in patients’ abnormal intestinal movements even with post-antibiotic decreased bacterial levels. It should be noted that varying antibiotics were used in the different studies.
These researchers suggest that colonic fermentation, and not bacterial overgrowth could be producing the gases that other researchers have measured. They also noted mildly increased levels of bacteria in the IBS group over the control group. While the study authors clearly did not see a causal relationship between SIBO and IBS, they do recommend further study.

