Eosinophilic Esophagitis Patient Journey
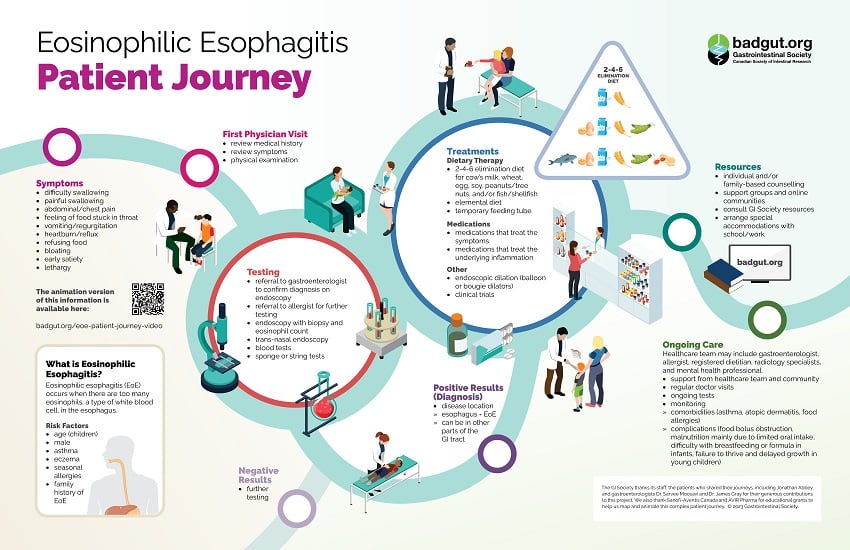
Eosinophilic esophagitis (EoE) occurs when there are too many eosinophils, a type of white blood cell, in the esophagus. The medical community knew little about this disease until the past few decades. In fact, scientists published the first report on EoE in 1978. Because it is so new and relatively rare, it can be time-consuming and difficult to get an accurate diagnosis. About 10 in 100,000 people are diagnosed with EoE each year. It is most common in children and adults 30-50 years of age, especially males, but can affect people of any age. Kids who have a family history of EoE, asthma, eczema, rhinitis, seasonal allergies, or a genetic tendency to develop allergic diseases, are more likely to develop EoE.
Symptoms of EoE can vary greatly between individuals. Sometimes there are symptoms in the esophagus that can make it easier to pinpoint EoE, such as difficulty swallowing, painful swallowing, the feeling of food stuck in the throat, and heartburn/reflux. One concerning symptom is food bolus obstruction, in which food completely blocks off the esophagus and an individual is unable to eat or drink. This is not the same as choking, as the patient can still breathe and talk normally, but it requires urgent medical attention if the person is unable to dislodge it through swallowing or coughing.
Other symptoms are more generalized and include abdominal/chest pain, vomiting/regurgitation, bloating, diarrhea, constipation, malnutrition due to inadequate food intake, feeling full quickly, and lethargy. Infants often have difficulties with both breastfeeding and standard formulas, and young children can experience failure to thrive and delayed growth. Children are less likely to experience symptoms in the esophagus.
Even before a diagnosis, on top of eliminating allergens, many patients make adaptations to what, how, when, and where they eat to manage their condition. The acronym ‘IMPACT’ outlines these behaviours:
Ingest fluids with meals,
Modify food (cutting into very small pieces, pureeing),
Prolong mealtimes,
Avoid hard texture foods,
Chew excessively, and
Turn away tablets/pills.
Some other methods include avoiding trigger foods, only eating food cooked at home, and packing food to eat while out.
Diagnosis begins with a visit to the doctor, who will review the patient’s symptoms and medical history. Many gastrointestinal conditions have symptoms in common, so the physician might conduct or order a number of tests to make a diagnosis, or refer the patient to a gastroenterologist to confirm diagnosis, or to an allergist for further testing. Some conditions that might need to be ruled out include gastroesophageal reflux disease (GERD), nerve damage in the esophagus (achalasia), Crohn’s disease with esophageal involvement, infections, connective tissue disorders, and drug hypersensitivity reactions. However, it is also possible to have these other conditions along with EoE. The path to a diagnosis can be frustrating and confusing, so it is important that you do not blame yourself for not being able to identify the patterns sooner.
General diagnostic assessments can include physical examination, blood tests, ultrasound, CT scan, MRI, and others. If the physician suspects EoE, then endoscopy with biopsy for eosinophil count will be performed. Trans-nasal endoscopy, and sponge or string tests could also be particularly helpful, if available.
To receive a diagnosis of EoE, an individual needs to have an eosinophil count of at least 15 eos/hpf on biopsy (or ~60 eos/ mm²). The high eosinophil count needs to be in the esophagus specifically, but high eosinophils in other parts of the digestive tract can indicate other forms of eosinophilic gastrointestinal disease, such as eosinophilic gastroenteritis when they are in the stomach/small intestine or eosinophilic colitis when they are in the colon.
Diagnosis is bittersweet for many people because, while they might feel relieved to finally have a name for their problem, the disease is very rare and there are few medications or other treatment options.
Once diagnosed, most patients and their families want to learn more about EoE. Support groups and online communities can help, as can resources from the GI Society. Some find that individual and/or family-based counselling is helpful, and some might need to arrange special accommodations with school or work while in the early stages of finding the right treatment until they have their symptoms managed.
EoE Patient Journey Video
EoE is a lifelong disease that requires ongoing maintenance therapy, and there are few options available right now. While there is no cure, treatments can significantly improve symptoms, induce remission, and lead to a better quality of life. Without treatment, inflammation can progress to permanent damage and esophageal remodelling, including esophageal stricture formation (narrowing of the esophagus).
Patients usually must start with dietary therapy, specifically the 2-4-6 step-up elimination diet to remove six common food allergens: cow’s milk, wheat, egg, soy, peanuts/tree nuts, and/or fish/shellfish. This involves removing the two most allergenic foods (dairy and wheat), then, if that doesn’t decrease eosinophils enough, removing the four most allergenic (dairy, wheat, eggs, and soy), and if that is still not enough, removing all six. This can be difficult, as the patient needs to do each step for at least eight weeks, followed by endoscopy and biopsy to check for eosinophils, for accurate results.
Some patients need to stop eating normal food completely and follow an elemental diet, which involves getting nourishment from a specialized amino acid formula. However, this formula has an unpleasant taste, so a person might even need a temporary feeding tube to consume it. The elemental diet is very restrictive and expensive. While it can be helpful temporarily, it is not a good long-term treatment option.
There are currently two medications approved by Health Canada to treat EoE. Jorveza™ (budesonide orodispersible tablet) is an oral medication that helps adults induce and maintain remission. Dupixent® (dupilumab) is a subcutaneous weekly injection that is available for those 12 years and older who weigh at least 40 kg (88 lb). Both treatments reduce inflammation in the esophagus, but they use different methods: Jorveza™ is a corticosteroid and Dupixent® is a biologic.
Some physicians will also prescribe other medications, such as swallowed topical corticosteroids adapted for the esophagus or proton pump inhibitors, but these off-label medications (not approved by Health Canada to treat EoE) can sometimes cause other digestive symptoms.
Another treatment option is endoscopic dilation (balloon or bougie dilators) in those with strictures, as it can stretch the tightened area out and make swallowing easier. There are also clinical trials for new treatments and medications ongoing, which will hopefully lead to more options down the line. Please consult your treating physician to find out if these options might be available for you.
Patients will need long-term support from their healthcare team and community, such as regular visits with a gastroenterologist and routine tests to monitor disease activity and check for complications. These can include malnutrition, anemia, and poor growth in children, as well as rare, more serious complications, such as esophageal stricture or obstruction, spontaneous esophageal perforation, or esophageal candidiasis. There is no evidence so far that EoE is a premalignant condition.
Since EoE often limits what a person can eat, registered dietitians can help make a diet plan that works with an individual’s limitations, requirements, and preferences. Exercise is also important to maintain body strength and improve overall wellbeing. However, it can be difficult to exercise consistently when ill, and there is also a risk of increasing symptoms such as chest pain or throat discomfort. Consult your physician on which exercises are best for you and how you can minimize risks. Some individuals with EoE might need to see an allergist, especially if they have comorbidities such as asthma, atopic dermatitis, or other food allergies.
Mental health care is also very important. EoE can have a massive impact on quality of life because the diet restrictions and painful symptoms can lead to social isolation and feelings of embarrassment. These issues can be particularly difficult for children and teenagers, who might need to eat away from other kids during lunch or miss out on parties and other activities involving food to avoid cross-contamination. Without proper psychological care, anxiety and depression can impact quality-of-life even more than EoE. Some things that can help include support groups and meditation, as well as seeing a counsellor, psychologist, or psychiatrist for more in-depth care.
While EoE requires long-term monitoring and support, it is possible to get the disease under control to the degree that you can live a healthy life free from symptoms.