Medication Supply Chain Video
Video Transcript
In Canada, we have access to a vast variety of medications from all over the world. However, their supply chains are complex and vulnerable to disruptions, which can lead to drug shortages and restrictions. This limits medicine options for injuries, infection, chronic diseases, cancer, and many other conditions.
Challenges became clearer during the pandemic, which caused disturbances to the supply chains that bring us masks, ventilators, and even toilet paper. However, the medication supply chain is much more complicated.
We can categorize this into four stages after drug discovery and development. These are regulatory approvals, manufacturing, procurement and distribution, and then frontline delivery to patients.
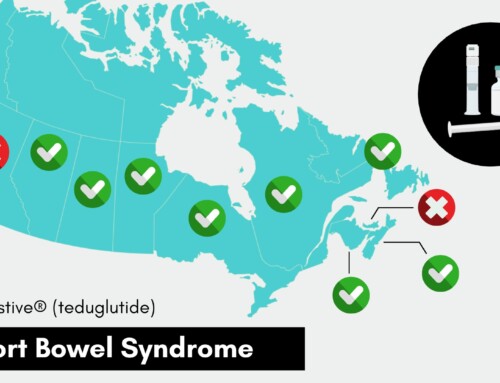
In the first stage, drug manufacturers submit their research on new drug discoveries to Health Canada for approval of a medication’s safety, efficacy, and quality to enter the Canadian market. Once approved, several other federal, provincial, and/or territorial agencies manage drug prices. Canada represents only 2% of the global market for medicines and continues to develop an increasingly complex regulatory landscape that can create extensive delays.
Canada strongly relies on international markets for drug manufacturing. Close to 70% of our prescription drugs come from foreign manufacturers, and about 90% of the medications we produce here require ingredients and raw materials from other countries.
With procurement and distribution, drugs originate from all over the world, eventually arriving at a pharmacy after a variety of other processes. These include packaging and labelling, storage and inventory management, purchase and sales transactions, refrigeration and quality control, utilities, lease, human resources, insurance, and transportation. All this is done using robust IT systems and precise skills to manage complex requirements for quality assurance and personal protection equipment.
Hospitals and health authorities often use wholesalers and specialized group purchasing organizations and associations to broker medications in bulk from distributors and directly from pharmaceutical companies.
At the final stage of the supply chain, healthcare professionals deliver and/or administer these medications to patients. The costs of resources and specialized services throughout the medication supply chain are part of drug prices.
International policies, border restrictions, and global crises, such as COVID-19, climate, and conflict, can all have significant impacts on our medication supply chain. Labour shortages in healthcare are another contributing factor, meaning that sometimes patients can’t even access a healthcare provider to obtain a prescription. Pharmacists are also scrambling to locate lower-cost alternatives to supplement medications that are in short supply.
Being such a small global player manifests several challenges for the medication supply chain in Canada. Costs are on the rise while changes in regulations drive prices lower, which can affect the attractiveness of the Canadian market for innovative medication supply. Despite inflation, healthcare funding throughout the system, especially for labour, remains critically low while workload increases, pressuring the supply chain to readjust and absorb the higher costs of goods and services without adjusted compensation. This could lead to further job losses, delays and reductions in deliveries, discontinued products, shortages, and decreased service for patients at the pharmacy and within patient support programs.
As our healthcare systems continue to strain, the federal government, along with the provinces and territories, must work together to ensure that Canadians have timely and affordable access to the care and medications they need. They must also strengthen efforts in attracting the latest international research and talent to the Canadian market and ensure that regulations and policies do not hinder access to innovative therapies.