Hidradenitis Suppurativa and its Connection to IBD
Inflammatory bowel disease (IBD) primarily refers to two diseases: Crohn’s disease and ulcerative colitis. These both involve inflammation in the gut, but in ulcerative colitis the inflammation is limited to the inner lining (mucosa) of the colon whereas in Crohn’s disease it can affect any part of the gut and can penetrate the full thickness of the intestinal wall. Symptoms include severe abdominal pain, frequent diarrhea, rectal bleeding, fever, nutritional deficiencies, and weight loss. Treatment is highly personalized and typically involves lifelong adherence to medications as well as dietary and lifestyle modifications, with some individuals requiring surgery.
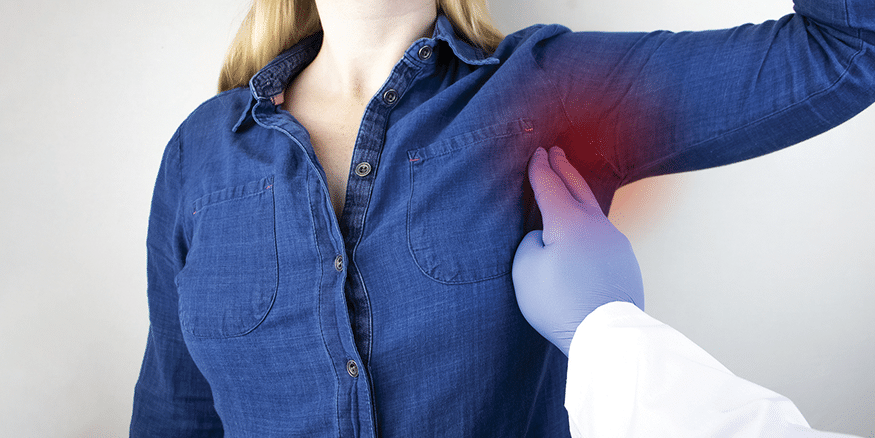
Hidradenitis suppurativa (HS) is a chronic, immune-mediated disease that causes boils on an individual’s underarms, groin, and/or under breasts. In mild cases, these are typically pimple-like, but they can worsen into recurrent abscesses and chronic lesions. The more severe stages of HS can be extremely painful and involve foul-smelling drainage and tunnel-like tracts under the skin. HS is more common in females than in males and can negatively affect self esteem and mental health. As with IBD, treatment varies between individuals and can include a combination of lifestyle changes, medications, and sometimes surgical procedures.
Both of these are inflammatory diseases; one of the gut and the other of skin follicles. They can reduce quality of life, especially as bowel problems and skin conditions tend to be taboo, meaning that those affected are not only experiencing devastating symptoms, they also often lack social support. To make things more difficult, many individuals who have one inflammatory disease are more likely to develop another.
A 2020 study done at Mount Sinai Hospital in Toronto looked into whether certain individuals with IBD were more likely than others to get HS.1 The authors cite previous research that shows the risk of HS is nine times higher in those with IBD than in the general population, and speculate that factors related to the immune system, genetics, and the microbiome might predispose individuals to both conditions.
The researchers compared 29 individuals with IBD and HS to 145 with IBD but no HS and looked for differences between the group. Those with IBD and HS weighed more than those with just IBD (82 kg vs 61 kg), which matches with past research that shows obesity is a risk factor for developing HS. However, this does not mean that being overweight causes HS, as it is an immune condition. Smoking tobacco also appeared to be a factor, as there were much higher rates of current (14%) or past (30%) smokers in those with HS compared to those without (2% current and 6% past smokers).
Looking at IBD-specific factors, HS was more common in those with Crohn’s disease than ulcerative colitis, especially in those with active perianal disease. It was also more common in those who had active endoscopic disease, which is the presence of active inflammation visible during a scoping procedure.
This was a fairly small study, but it builds on the growing body of evidence involving the association between IBD and HS. If you have IBD and are concerned about boils or pimples in areas where you grow hair, particularly in the groin or underarm regions, then speak with your healthcare team. While HS is still rare, those with IBD, especially those who have the risk factors identified above, are more likely to develop the disease than those without IBD. HS is a progressive disease, so beginning treatment early is key.
For more information about hidradenitis suppurativa, go to www.hsheroes.ca. HS Heroes is a community for people living with HS dedicated to increasing awareness, educating, and advocating for those whose lives have been affected by the disease, whether a patient, family member, friend, caregiver, or healthcare professional.

