Click here to download a PDF of this information.
Obesity
 Obesity is a multi-factorial, chronic, relapsing disease that occurs when a person has an abnormal or excessive accumulation of body fat (adipose tissue) leading to an increased risk of health complications. Over the past few decades, obesity has grown in prevalence in Canada and other developed nations. Several health organizations, including the Canadian Medical Association and the World Health Organization, classify obesity as a chronic disease. The European Union Commission has listed obesity as one of the high-risk groups who are medically vulnerable.
Obesity is a multi-factorial, chronic, relapsing disease that occurs when a person has an abnormal or excessive accumulation of body fat (adipose tissue) leading to an increased risk of health complications. Over the past few decades, obesity has grown in prevalence in Canada and other developed nations. Several health organizations, including the Canadian Medical Association and the World Health Organization, classify obesity as a chronic disease. The European Union Commission has listed obesity as one of the high-risk groups who are medically vulnerable.
Intricate factors contribute to causing obesity, including biology, environment, psychology, and lifestyle. Excessive amounts of body fat can affect your health. However, treatment is so much more complex than the commonly misused rhetoric of eat less and move more, and it involves lifelong management using various treatment modalities.
There are a variety of tools that can mitigate weight gain. You will need to use them together and they will stop working once you stop using them. We will get into those methods below.
Diagnosis and Classification
We will first review the established diagnosis process and then share how this is evolving as experts learn more about obesity. To diagnose obesity, your physician will measure your weight and height to calculate your body mass index, or BMI. They might also measure your waist circumference since a high concentration of body fat in the abdominal region carries a higher risk than fat in other parts of the body.
Body Mass Index
In the 1830s, Lambert Adolphe Jacques Quetelet, a Belgian astronomer, mathematician, statistician, and sociologist, developed a simple math formula while studying what made the average man. It was not meant to be used as a medical tool. More than a century later, health professionals looking for a simple method to calculate whether someone was underweight, healthy, or overweight, settled on this calculation and started calling it the BMI.
You can calculate your BMI by dividing your weight in kilograms by your height in metres squared. For example, someone who weighs 80 kg (176 lbs) and is 1.75 m (5’9”) tall would have a BMI of about 27 (80/1.752). Medical experts define overweight as a BMI of 25-29.9 kg/m2 and obesity as a BMI of 30 kg/m2 or greater. There are also several categories of obesity severity (see chart).
Using this formula, the higher your BMI, the greater your risk is of developing obesity-related conditions. If you have a BMI greater than 40 (class III obesity), then you are at the greatest risk.
BMI Calculator
| Underweight | <18.5 |
| Normal/Ideal weight | 18.5-24.9 |
| Overweight | 25-29.9 |
| Obesity Class I | 30-34.9 |
| Obesity Class II | 35-39.9 |
| Obesity Class III | ≥40 |
BMI Flaws
BMI is simple to calculate, but this is because it does not consider many important factors, such as overall fat or lean tissue (muscle) content, or the different levels of adiposity based on age, physical activity, ethnicity, and sex. The World Health Organization states, “…it is expected that [BMI] overestimates adiposity in some cases and underestimates it in others.”
You might have a BMI that indicates overweight or obesity but have a healthy level of body fat and an ideal waist measurement, and thus you would not technically have obesity. This typically occurs in individuals who have a larger proportion of muscle mass, such as some professional athletes.
On the other hand, having a normal/ideal or overweight BMI does not necessarily mean that you do not have obesity. Sometimes, a physician might still diagnose a person who has a BMI less than 30 kg/m2 with obesity, such as those who accumulate more weight in the abdomen or those of certain ethnic backgrounds. For example, research shows that persons of Chinese ancestry tend to experience greater rates of adverse health conditions at lower BMIs than those of European ancestry. Researchers suggest a BMI greater than 25.9 kg/m2 in men and 26.6 kg/m2 in women could indicate obesity in this population. Canadians with East or South Asian ancestry might have obesity at these lower cut-offs.
Beyond BMI
The emerging method for diagnosing obesity is to measure your health, but not in numbers such as the BMI. This involves looking at your weight in the context of its effect on your health. For example, a physician will assess whether you have diabetes, high blood pressure, heart disease, polycystic ovary syndrome, anxiety, depression, or other health conditions.
Obesity Video
Statistics
In 2018, Statistics Canada released a document containing figures about obesity in this country. They found that 26.8% of those who were 18 years of age or older had obesity, and another 36.6% were overweight. Overall, 63.1% of participants had a weight above the ideal range. They found higher rates of obesity in men (69.4%) than in women (56.7%). There was quite a variance in obesity rates by province, with the lowest being 23.1% in British Columbia and the highest being 40.2% in Newfoundland. The survey data also showed that those with obesity are more likely to have certain medical conditions than those of an ideal weight, including type 2 diabetes (13.4% in those with obesity vs 2.9% in those with an ideal weight), high blood pressure (29.5% vs 9.5%), and heart disease (6.0% vs 2.7%).
A study that pooled data from 20 others found that obesity reduces life expectancy by about 6.5 years for individuals with a BMI of 40-44.9, and 13.7 years for those with a BMI of 55-59.9.
Causes of Obesity
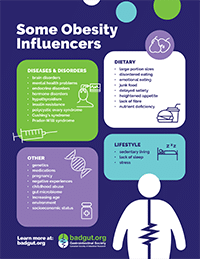 The causes of obesity are complex and multifaceted and include interactions among multiple genetic and environmental factors. While excess food intake combined with inadequate exercise is the go-to explanation for obesity, it is an over-simplification and does not address the complex underlying reasons why weight gain occurs. Genetics, medications, poor sleep (including from sleep apnea), stress, trauma, mental health problems, socioeconomic status, hormones, endocrine disorders, binge eating disorder, and more can all influence the development of obesity. More than a hundred different genes are factors in overweight and obesity and scientists are still learning how they influence the body. We do know that they contribute to the causes of obesity in many ways, such as by affecting your appetite, sense of fullness (satiety), metabolism, food cravings, body-fat distribution, and the tendency to use eating to cope with stress. Some studies show that your parents’ and grandparents’ lifestyles can affect your body’s way of interacting with food. To an extent, even what your mother ate during her pregnancy with you can affect your weight as an adult.
The causes of obesity are complex and multifaceted and include interactions among multiple genetic and environmental factors. While excess food intake combined with inadequate exercise is the go-to explanation for obesity, it is an over-simplification and does not address the complex underlying reasons why weight gain occurs. Genetics, medications, poor sleep (including from sleep apnea), stress, trauma, mental health problems, socioeconomic status, hormones, endocrine disorders, binge eating disorder, and more can all influence the development of obesity. More than a hundred different genes are factors in overweight and obesity and scientists are still learning how they influence the body. We do know that they contribute to the causes of obesity in many ways, such as by affecting your appetite, sense of fullness (satiety), metabolism, food cravings, body-fat distribution, and the tendency to use eating to cope with stress. Some studies show that your parents’ and grandparents’ lifestyles can affect your body’s way of interacting with food. To an extent, even what your mother ate during her pregnancy with you can affect your weight as an adult.
Persons who are living with obesity often report that their cravings for food never go away. They could eat a large meal and when others might feel too full to move, the systems in their body are still signalling that they need to eat. This is a fundamental need of the body that is almost impossible to ignore and is a major element contributing to weight gain. In addition, some people might be surprised at the massive difference in calories required for people depending on their age, height, sex, and activity level. This means that someone with obesity could eat less food than someone who is thin and feel like they must eat next to nothing to lose weight.
Complications
While the only actual symptom of obesity is increased body fat, particularly around the abdomen, health complications can arise from this disease. Excess weight influences human physiology in diverse ways, which can range from excess pressure on the joints and in the abdominal region to hormonal effects, since adipose tissue can lead to increases in certain hormone levels. Individuals with obesity are at an increased risk for a wide range of conditions, but these conditions can also occur in those who are underweight or an ideal weight:
- insulin resistance
- type 2 diabetes
- high blood pressure
- heart disease
- stroke
- gout
- sleep apnea
- osteoarthritis
- headache or migraine
- endocrine conditions (e.g., polycystic ovary syndrome)
- infertility
- diminished sex drive
- mental health problems (e.g., low self-esteem, anxiety, depression)
- reduced quality of life
- skin problems
- hirsutism
- phlebitis
- kidney disease
- gynecomastia
- certain types of cancer (e.g., breast, cervical, uterine, prostate, colorectal)
- digestive conditions (more information on this topic is on our website)
Women with obesity also have an increased risk of complications during pregnancy, such as blood clots, preeclampsia, gestational diabetes, and miscarriage, and their babies are at a higher risk of being born with certain birth defects or being born premature.
Obesity can complicate surgeries as you are more susceptible to infections, and you might heal more slowly. Accurately calculating anesthetic dosage for a person with obesity can also pose challenges. Obesity is also a risk factor for complications from COVID-19.
Management and Treatments
The first line of treatment for obesity typically involves dietary and lifestyle changes. However, obesity is a chronic disease, which means that just losing weight does not cure it. It typically involves a life-long effort to combat regaining lost weight or gaining more weight. Other treatments are available, including medications, cognitive therapy, and surgery. Most persons with obesity will need to use more than one treatment modality at any given time and over the course of their lifetime.
Where there is an underlying cause of obesity, treating this can lead to weight loss. For example, if you experience rapid weight gain after switching to a new medication (such as corticosteroids, which are highly associated with weight gain), you might find it easier to lose weight if your physician switches you to a different medication. Someone who is experiencing weight gain due to an endocrine condition might find it easier to lose weight once that condition is under control.
Along with trying to manage weight, treatment can focus on reducing the effects of obesity, such as balancing blood sugar if the person has type 2 diabetes.
Diet
We all know that it is important to maintain proper dietary habits and we recommend following Canada’s Food Guide. However, if you have an obesity diagnosis, it’s not necessarily that simple. Studies show that the human body is possessive of the weight it gains, and it will do everything it can to resist weight loss. This is the basis of the obesity battle.
The primary target for treating obesity is stopping weight gain, followed by weight loss. Food education, such as knowledge of the calorie content, nutrient density, and satiety index of different foods can be helpful for some individuals. Dietary treatment plans involve reducing calorie intake and increasing exercise (also known as maintaining a caloric deficit). A variety of different caloric deficit plans are available and can range from reducing portion sizes to diets that involve cutting out entire food groups, and these vary in effectiveness.
We are not here to discourage you if you want to embark on a new diet to lose weight. However, the evidence does show little benefit from dieting over the long-term. For example, in one American study, three years after participants concluded a weight loss program, only 12% had kept off at least 75% of the weight they had lost, while 40% had gained back more weight than they had originally lost. Weight loss camps are a commercial approach in treating severe obesity. However, results from Denmark demonstrate that even in a multidisciplinary, intensive setting that focuses on diet, exercise, and psychological counselling, only 28% had maintained a weight loss above 10% after 4 years. This emphasizes that obesity is a chronic condition that needs additional strategies to a diet plan in the effort to maintain a sufficient weight loss.
A nutritious, balanced diet is important for everyone, but no specific diet is the secret to cure or manage obesity. Studies that show poor outcomes often focus on restrictive diet routines. These can be difficult to maintain as they often lead to strong cravings for ‘forbidden’ foods and can interfere with day-to-day life. In addition, restricting calories too heavily causes hormonal changes that increase your hunger and appetite (see Hunger and Appetite on our website).
Following a balanced approach to eating by gradually reducing portion sizes and focusing on nutritious foods is more effective than drastic changes such as removing multiple food groups. However, these simple dietary changes tend to cause slow, gradual weight loss, which can be discouraging in the short term.
It can be difficult to maintain a caloric deficit, even when following a well-balanced diet. Hormonal changes and certain medications can also drastically increase appetite and it is common for people to fall back into old eating habits. This is why, despite this being a seemingly simple solution, obesity rates are continuing to grow.
All of us can benefit from employing mindful eating habits, which is about using mindfulness to reach a state of full attention to your experiences, cravings, and physical cues when eating. This involves techniques such as eating slowly and without distraction, listening to physical hunger cues, and eating only until you feel full.
For more information on diet, and to get help creating a diet plan that works best for your individual preferences and lifestyle, contact a registered dietitian.
The Canadian Adult Obesity Clinical Practice Guidelines: Commercial Products and Programs in Obesity Management rates these programs as helpful for achieving mild to moderate weight loss when followed for the short- and medium-term: WW® (Weight Watchers), Optifast®, Jenny Craig®, and Nutrisystem Inc.
Crash Diets Fail Long-Term
Despite the extensive marketing and apparent commercial success of drastic weight loss programs that promote restrictive diets, including the type, nature, and amount of food you consume, these programs do not provide long-term success. They often put the person in a worse condition than they were before they started the program, including a big hit to their finances!
While sensational entertainment shows, such as The Biggest Loser, might give you hope, the reality is that you cannot sustain the diet and exercise routines that these contestants follow. They might experience rapid weight loss while a team of experts is helping them, but as soon as they return to the real world, it is exceedingly difficult to maintain these changes. Rapid weight loss from crash dieting can cause hormonal changes that drastically increase appetite and reduce the number of calories that your body burns at rest.
A 2016 study from the US National Institutes of Health (NIH) followed fourteen former The Biggest Loser contestants and found that thirteen of them regained a significant portion of the weight they lost on the show. Four were heavier in 2016 than they were before they set foot on the set. When it comes to weight loss through dieting, most people have better success keeping the weight off by making incremental changes and gradually losing weight.
Exercise
While exercise on its own is often not sufficient for sustained weight loss, when practiced in tandem with a diet plan, it can increase chances of success. Exercise can improve conditions associated with obesity even without weight loss. These benefits include improving cardiovascular function and reducing blood pressure, improving blood sugar levels, maintaining muscle tone, improving lung function, reducing stress, and increasing the number of calories the body burns at rest. You might see better health results from low-impact exercise, including walking, swimming, and yoga.
It is important to note that any movement is exercise. If you move more than you have before, then that is progress, which can positively affect your health. Start small and focus on what makes you feel better. The adage, “no pain, no gain” is simply wrong. You should try to find something you enjoy so that you will be more likely to stick to it.
A kinesiologist might be able to guide you through a movement plan that works for you. These healthcare professionals study the principals of prevention, management, and performance related to human movement.
Just twenty minutes of energetic walking a day will start to shift the dangerous internal fat.
Support Systems
When it comes to success with dietary changes and physical activity, having a solid support system is vital. If you spend time with others who are constantly eating junk food and trying to make you join them, or who belittle you for trying to improve your health, it is difficult to stay on track. If you can gather support from the friends and family members who will help you succeed – the ones who will share healthy recipes and go for walks with you, or at least encourage you and be there for you when you need them – it can make a world of difference. They should be the kind of people who won’t monitor your actions and judge you, but who will simply support your choices.
Sleep
There is some evidence that a lack of sleep can lead to obesity by changing hormone levels, increasing appetite, and decreasing willpower. Ensuring you get enough sleep can help make it easier to manage weight by stabilizing hormone levels and giving you the energy you need to maintain an exercise regimen. Discuss this with your physician, who might send you for sleep tests to rule out sleep apnea.
Stress and Mental Health
Similarly to lack of sleep, stress can influence certain hormones that can lead to increased weight. Chronic stress can lead to the production of cortisol, which can increase appetite and lead to weight gain around the abdomen. You might turn to ‘comfort foods’ when feeling stressed, depressed, anxious, isolated, or even bored. These foods are typically high calorie and low in nutrients. Managing emotional eating can be challenging. Whether you eat for emotional reasons because of an underlying condition or from occasional stressors, learning alternative strategies to manage these feelings can help reduce your desire to overeat.
If you are feeling angry, anxious, or upset, finding positive coping mechanisms can help blow off steam and keep your mind from wandering; try learning a new sport, hiking in nature, or just going for a walk while listening to music or an audiobook. If you are eating due to loneliness or feeling down, calling a friend or joining an online forum might make you feel better. If you find yourself eating too much because you are bored, try taking up a hobby. Things such as knitting, crocheting, drawing, painting, origami, scrapbooking, or doing yoga can keep you busy while you relax at the end of the day. If you are feeling stressed, any of the above can help, as can focusing on relaxing: have a nice hot bath, curl up with a good book and a hot drink, or watch a funny movie.
You could also consider a licensed cognitive-behavioural program for emotional eating, which vary in availability across the country.
Journaling can help. You might find that writing out in long form how you are feeling can reduce stress and bullet journaling can help you better understand your triggers. Tracking what and when you eat, along with data on how much sleep you get, whether or not you exercised, your general emotional state, and how stressed you were on a given day might help you identify which habits and patterns improve your mental health and which make it worse. We have created a Digestive Health Journal you might find helpful, which is available on Amazon.
If you frequently experience symptoms of depression or anxiety, or if you are concerned about your mental health, please contact your physician.
Medications
There are prescription medications available to treat obesity in Canada, using different mechanisms of action. No medication can work entirely on its own to manage obesity, but they might make it easier for you to adhere to a weight-loss plan. It is still necessary to work on lifestyle changes, such as increasing exercise and improving your diet, while you take any of these medications. Health Canada has approved medications to treat obesity for use in anyone with a BMI ≥30 or anyone with a BMI ≥27 who also has a weight-related disease (e.g., controlled hypertension, type 2 diabetes mellitus, or dyslipidemia).
The combination of naltrexone and bupropion (Contrave®) works by supressing appetite by affecting two areas of the brain involved in the regulation of food intake. It is available in pill form, starting with a once-daily dosage and increasing gradually to a maintenance dose of two pills twice daily. Contrave® is generally a well-tolerated medication, with nausea being the most common side effect. Your physician might check your blood pressure and heart rate prior to starting this medication to ensure it is appropriate for you and will monitor these regularly.
Liraglutide (Saxenda®) and semaglutide (Wegovy®) work by regulating your appetite level. You self-administer these medications via injection under the skin (subcutaneously) daily or weekly, depending on the product. To reduce the risk of side effects, it is important to start at the prescribed initial dose and gradually increase to the maintenance dose. Side effects of these medications most commonly include gastrointestinal adverse effects such as nausea and diarrhea, which usually disappear after a few days or weeks. They can also cause low blood sugar, headaches, and dizziness. In very rare cases, patients might experience pancreatitis, gallstones, or gastroparesis.
Orlistat (Xenical®) inhibits lipase, an enzyme that breaks down dietary fat into absorbable components. When you use this medication, your body is unable to absorb the fats and all its subsequent calories, eliminating them with your bowel movements. Side effects can include diarrhea, oily stools, oily discharge when passing gas, and bowel urgency.
While there are over-the-counter supplements marketed as weight loss aids, the majority have little evidence of efficacy and some of them can even be dangerous. It is best to avoid these unless your physician recommends you take a specific product. You may also speak with your pharmacist about these prescription or non-prescription therapies.
Bariatric Surgery
There are surgeries available to treat obesity. Our website covers a more detailed examination of this topic, which we have condensed here. Surgery typically works by:
- reducing the amount of food that the stomach can hold, thereby making it difficult to consume enough calories to maintain bodyweight, and/or
- changing the path that food takes during digestion to avoid parts of the small intestine, which reduces absorption of some nutrients, including calories.
Most physicians won’t recommend weight loss surgery unless you have a BMI ≥40 or a BMI ≥35 along with weight-related health complications (e.g., type 2 diabetes, heart disease, sleep apnea) and have already failed to lose weight using less invasive options, such as lifestyle modifications and medications. Physicians rarely recommend bariatric surgery for anyone younger than 18 years of age.
Here are the more common forms of bariatric surgery:
Gastric Sleeve: a surgeon will remove part of your stomach, leaving just a thin sleeve, approximately the size of a small banana, behind. This method simply reduces the amount of food you can eat during a window of time.
Gastric Bypass: a surgeon removes part of the stomach, leaving just a small pouch, and then connects the small pouch to the middle of the small intestine. Roux-en-Y is another name for this process. This surgery works in two ways: you can’t eat as much because the stomach is smaller, and your body won’t absorb as many calories because of the small intestine bypass.
Gastric Band: a surgeon will place a band around the upper part of the stomach to create a smaller pouch. The surgeon can adjust the band to make the available stomach area smaller or larger, as needed. However, due to poor results, this is not widely recommended anymore.
Intragastric Balloons: this is a newer and less common form of surgery at this time. It is a temporary measure that involves placing a fluid-filled balloon into the stomach that delays the rate of gastric emptying. It is different from other methods of surgery as it does not involve modifying the structure of the digestive tract and it is reversible, but it still has risks.
Bariatric surgery is highly effective, often leading to significant weight loss and reversal of several obesity-related diseases, such as type 2 diabetes and high blood pressure. However, it is not without risks. Of those who have bariatric surgery, 5% experience complications while in hospital and 6% need hospital readmission within a month of release due to complications. The mortality rate for bariatric surgeries is between 0.1-2%.
There is growing evidence of potentially severe – occasionally even life-threatening – nutritional and pharmacological consequences of bariatric surgery, including iron deficiency anemia.
Please note that some types of surgery you might have heard of, such as liposuction and body sculpting, are not effective forms of weight loss. These focus on minor changes to the body and are not treatments for obesity.
Side Effects of Weight Loss
For a person who has lived with obesity for a long time, and who manages to lose significant weight, new issues can arise. As the body uses fat stores, the stretched skin relaxes but there is usually not sufficient elasticity for it to resume its pre-weight-gain form. Loose skin can happen to anyone, but it is a more common consequence for those who:
- are older when they lose weight
- lose weight very quickly (more than 0.5-1 kg [1-2 lbs] per week)
- lose more than 45 kg (100 lbs)
- do not exercise while losing weight
Patients might require surgery to remove this excess skin, but most public plans will not cover this, as they consider it cosmetic. We believe that public plans should cover these surgeries, as a unique set of health problems can arise from excessive amounts of loose skin, such as excessive sagging, chafing, and sores between the folds that are difficult to heal.
Living with obesity negatively affects mental health. After going through treatment that effectively reduces body weight, you might still have the consequences of excessive weight, which can further affect mental health.
Rapid weight loss can also lead to gallstones. This is because the liver secretes more cholesterol into the bile to help deal with the extra fat the body is breaking down. Losing weight slowly can help prevent the formation of gallstones.
If you are making drastic changes to your diet, nutrition deficiencies are possible, such as iron, vitamin B12, or vitamin D deficiency. You might also experience periods of low blood sugar. The changes to your body when you eat at a deficit can cause many symptoms, including fatigue, irritability, dizziness, headaches, hormonal changes, constipation, and hair loss. If you experience these symptoms while losing weight, speak with your physician.
However, it is important to note that in the case of weight loss, the benefits are greater than the risks. You can reduce your chances of experiencing negative effects of weight loss by working with your healthcare team to establish a routine that focuses on slow, steady, and sustainable weight loss and adequate nutrient intake.
Outlook
Claims that you can easily treat obesity through simple lifestyle changes are harmful and reinforce social stigma. These are also in stark contrast to the conversation around other diseases, none of which have simple solutions. We need to work together on reducing the social stigma that permeates all levels of society, so those living with obesity get the same respect and attention as others accessing healthcare. Just as for other chronic diseases, medical intervention will be necessary.
Untreated obesity can lead to complications, increase the risk of other medical conditions, and decrease quality of life. It might be easier to prevent obesity, but even this is complex. There are many treatment options available, each with a distinct set of pros and cons.
Engage in ongoing dialogue with your physician about what treatments will be appropriate for you. Success can look different in each case. While, for now, the ideal target is to reach a healthy BMI, research shows that when individuals diagnosed with obesity lose just 5-10% of their body weight – e.g., 7-14 kg (15-30 lbs) in someone who weighs 140 kg (300 lbs) – it can help reduce the risk of weight-related conditions.
There are hurdles to overcome, but it is a good thing to strive for a manageable treatment plan that can help you lose enough weight to improve your health.
Want to learn more about obesity?
We have several related articles that may be helpful:
- Obesity
- Obesity Video
- Obesity Journey Video
- Obesity Journey Survey Report 2024
- Obesity Survey Results 2021
- Obesity Medications
- Bariatric Surgery
- Hunger and Appetite
- GI Issues Associated with Obesity
- Marty Enokson’s Battle with Obesity
- Don’t Blame the Patient