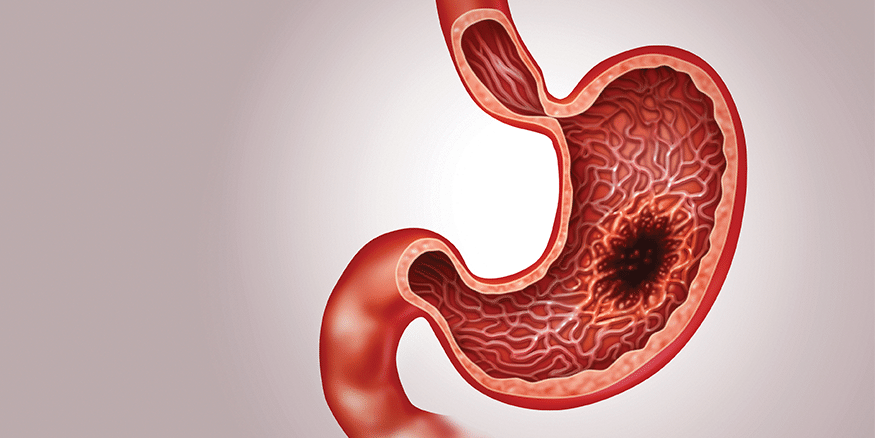
Stomach Cancer
Gastric cancer, more commonly known as stomach cancer, is an umbrella term that refers to several cancers originating in the stomach. In this article, we focus on gastric adenocarcinoma, which is a type of cancer that develops from the glands in the lining of the stomach. It makes up about 90% of all stomach cancers.1 Other stomach cancers include gastrointestinal (GI) stromal tumours and neuroendocrine tumours, which is a rare disease that originates in the GI tract and lungs.
Gastric cancer has a high global incidence rate compared to other cancers. However, the adoption of public sanitation, clean water supplies, and improvements in food production, processing, preservation, and hygiene have significantly contributed to the decline of gastric cancer.
Types of Gastric Cancer
Gastric adenocarcinoma consists of two subtypes called cardia gastric cancer and non-cardia gastric cancer.1 Cardia gastric cancer develops near the gastroesophageal junction, where the lower part of the esophagus attaches to the stomach. This subtype is associated with obesity, gastroesophageal reflux disease (GERD), and tobacco smoking. Cardia gastric cancer has worse long-term survival rates than non-cardia gastric cancer.
Non-cardia gastric cancer occurs in the main area of the stomach. It is associated with Helicobacter pylori (H. pylori) infection, tobacco smoking, and a diet with high salt consumption. H. pylori is a bacterium that infects stomach tissues that can cause stomach ulcers and, in rare cases, lead to gastric cancer. The source of the bacteria is not known but research suggests it is from food or water ingestion. H. pylori infection is generally chronic, and most people are not aware of the initial exposure, but blood and saliva tests are available for diagnosis. While it remains unclear how H. pylori contributes to the development of cancer, it accounts for nearly 90% of non-cardia gastric cancer cases worldwide.2
Clinicians also categorize gastric cancer by intestinal, diffuse, and indeterminate type. This classification focuses on its molecular and epidemiologic features. Nearly 3% of gastric cancer cases are hereditary diffuse gastric cancer (HDGC), which develops from a mutation of the CDH1 (epithelial cadherin) gene. Men who have the CDH1 gene mutation have an increased risk for HDGC by 70% while women have a 56% risk.3 Mutations in closely related genes are also associated with HDGC. If you have a family history of gastric cancer, speak with your doctor about options for genetic testing.
| Risk Factors | Cardia | Non-Cardia |
| age (60+ years old) | yes | yes |
| male | yes | yes |
| tobacco smoking | yes | yes |
| race | yes | yes |
| family history | yes | yes |
| low physical activity | yes | yes |
| low fibre intake | yes | yes |
| radiation | yes | yes |
| Helicobacter pylori | no | yes |
| high intake of salty and smoked foods | no | yes |
| low consumption of fruits and vegetables | no | yes |
| obesity | yes | no |
| GERD | yes | no |
Adapted from Karimi et al. 2
Symptoms
It is difficult to get an early diagnosis of stomach cancer because its symptoms are similar to those found in other diseases of the GI tract, including loss of appetite, heartburn, persistent indigestion, nausea, vomiting, and unexplained weight loss.
Diagnosis and Screening
Studies recommend screening only certain populations for gastric cancer in Canada. These include older individuals with a history of chronic gastric atrophy, pernicious anemia, gastric polyps, and partial gastrectomy.2 A physician may conduct an upper GI endoscopy (gastroscopy) to confirm your diagnosis. If you believe you may be at risk, contact your doctor.
Management
Managing gastric cancer will vary depending on your cancer stage upon diagnosis. Your healthcare team may provide patient supports for symptom management and palliative services. Your specialist may also recommend a gastroscopy after treatment to monitor side effects and look for signs of recurrent disease.4
Prevention
Eradication of H. pylori can reduce your risk of developing gastric cancer by 35%.2 There are many treatments available to eliminate H. pylori and all have in common a combination of two antibiotics in high doses plus other agents.
Dietary and lifestyle modifications can also lower your risk for gastric cancer. Smoking cessation and reducing your exposure to cigarette smoke are important to consider. People who currently smoke have a 25% increased risk for gastric cancer.5 Studies also show poor survival outcomes since smoking may lead to other cancers and complications. Using a hookah to smoke tobacco products is also associated with a higher risk for gastric cancer. The effects of vaping are not yet clear.
You should consume a balanced diet with fruits and vegetables and avoid excessive amounts of alcohol. The Mediterranean diet, with a high intake of fibre, combined with exercise, can also lower your risk and improve overall health.2 A recent literature review of articles published in English and Persian languages on the epidemiological aspects of gastric cancer in Iran found that there is a direct link between gastric cancer and a high intake of foods filled with preservatives.6 This includes the consumption of processed red meats, dairy, smoked meats, pickled vegetables, and salt.
If you have other medical conditions, consult your healthcare team on how to best achieve a healthy diet and an appropriate exercise regimen.
Don’t delay treatment during the pandemic!
Delaying cancer treatments by only four weeks can lead to worse outcomes, quality of life, and even death.7 While healthcare systems have experienced significant pressures due to COVID-19, they have adopted measures so that they can continue providing care safely and effectively. Follow the advice of the Public Health Officer in your community, such as wearing a mask, practicing physical distancing, and/or limiting your bubble to your household members. Let’s all work together to keep each other safe.
You may feel hesitant to reach out to your healthcare team when symptoms first appear. We, along with patient groups and healthcare organizations across the country, encourage Canadians living with cancer who have had their treatments paused, and those experiencing possible symptoms or have missed routine checks, to contact their doctor to get the care they need. Cancer doesn’t wait, so neither should you. Contact your healthcare team. Get checked!

