Ulcerative Colitis Patient Journey Video
Video Transcript
If you or a loved one have received an ulcerative colitis diagnosis, you might feel overwhelmed and concerned. The patient journey can be long and complex, but with the right tools and a support system, you can lead a healthy and balanced life.
Typically, the journey starts with symptoms that might include a combination of diarrhea, bowel urgency, incontinence, abdominal pain, cramping, fever, rectal bleeding, anemia, nausea, and vomiting. You might even avoid eating because of how much it hurts going through your system, or avoid going out because you are worried about your bowel habits. These can appear at any age, often beginning in children, young adults, or even middle age. Symptoms can be relentless, embarrassing, and scary.
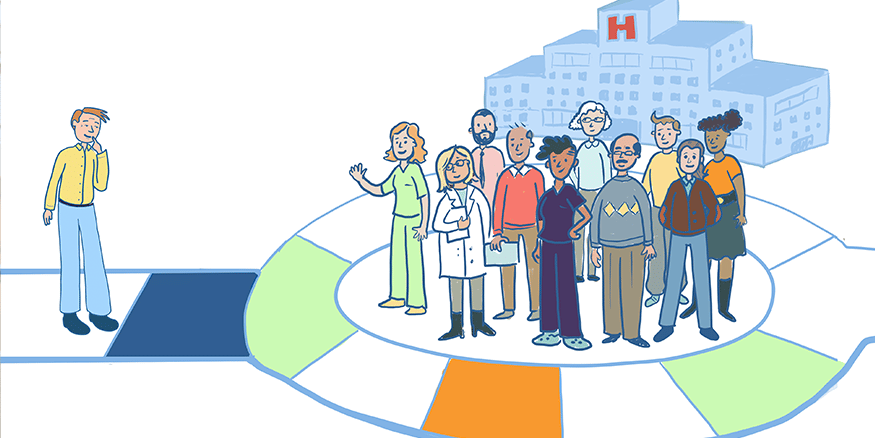
After experiencing these symptoms, which can be severe and greatly affect quality of life, most people visit a general practitioner, or GP, who will typically review your medical history and symptoms, perform a physical examination, and request some tests. There are many conditions that cause symptoms similar to those of ulcerative colitis, so the diagnosis could take years to pinpoint. These delays can be frustrating and overwhelming to live through. Usually, if symptoms don’t resolve, a GP will refer you to a gastroenterologist.
Assessments that can help a doctor zero in on an ulcerative colitis diagnosis and monitor disease state include blood tests (c-reactive protein, therapeutic drug monitoring, hemoglobin, etc.) and stool tests for biomarkers (calprotectin and lactoferrin) and for intestinal pathogens (e.g., C. difficile, parasites, etc.).
Ulcerative colitis starts at the rectum and increases in a continual pattern through the colon.
It presents uniquely in each person, so a diagnosis can differ by its severity such as mild, moderate, severe, or sudden and severe, and by its extent into the colon. This can be proctitis, left-sided colitis, or extensive colitis, also known as pancolitis. Ulcerative colitis affects only the mucosal lining of the colon.
It is easy to detect with a sigmoidoscopy or colonoscopy, as these allow the physician to look inside the colon for visual signs of inflammation and to remove tissue samples for testing.
Learning about this chronic disease can take a while. In some cases, you might have a physician who provides you with many resources, whereas others might have to seek various reliable printed or web educational resources, support groups and online communities, and individual and/or family-based counselling. The GI Society has many resources, including varied educational information and a support group.
With so many different forms of medications available, ulcerative colitis treatment looks different for each person. Medications play a vital role and will include ongoing anti-inflammatory medications and symptomatic medications from time to time. You may have to try several different medications until you find one that works and then, over time, you might need to change the medication again or change the dose. Certain side effects might make a drug unsuitable for you, so your doctor will change your medicine. Finding the right treatment is an ongoing process.
Since ulcerative colitis only involves the large bowel, removing this organ will remove the disease, but it is not a cure. Removing the colon can lead to other symptoms and complications and will require an ostomy. This involves a surgeon removing all or part of the colon, then bringing the end of the remaining intestine through a surgical opening in the abdominal wall, to which the patient can attach a removable appliance to collect stool. An ostomy may be either temporary or permanent, depending upon the situation.
Even with all of these treatment options, new symptoms might appear, severity might increase or decrease, so changes might need to be made to medications, or new assessments are needed. It can be a network of snakes and ladders!
Caring for ulcerative colitis consists of a comprehensive healthcare team, and this can include a gastroenterologist, nurses, registered dietitian, patient support program, mental health care professional, dermatologist, kinesiologist, ophthalmologist, rheumatologist, neurologist, and sometimes a visit to the hospital emergency. You will need routine tests to monitor disease activity and medication side effects. However, many patients experience flares, during which inflammation and symptoms return. At this point, more testing is necessary and treatment plans will need adjusting. Revisiting all the tests can be frustrating, but they are essential to ensure your body is healing.
Some patients need to arrange special accommodations with school or work. Some might need financial support as it can be difficult to work in severe cases, and they might need help to cover their medicine costs. It is important to find mental health support throughout your journey.
Remission is the goal, and this occurs when inflammation in the colon is reduced or resolved, and symptoms are minimal or gone.
Your journey might be worsened during difficult times when access to healthcare is strained. While the journey is long and complex, we hope you can find solutions that manage your condition.