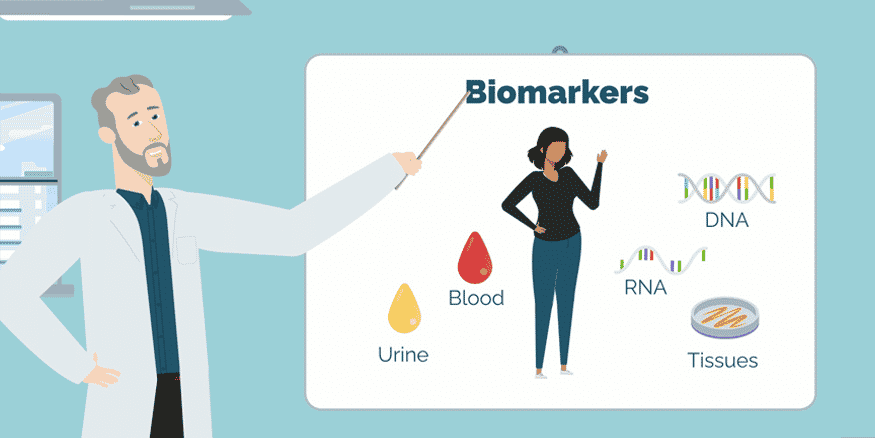
Biomarkers Video
Video Transcript
The human body contains chemical signatures, called biomarkers, in DNA, RNA, blood, urine, and all tissues. These can tell us valuable information about our health. Simply put, the results a healthcare professional gets from the laboratory after you go for a test can signal that all is well or that something is wrong. Biomarkers can also predict your risk for a disease or reveal how your body is responding to a treatment.
Using biomarkers, healthcare teams can customize tools and therapies to an individual’s biology. Biomarker research continues to expand, especially on how we can use them to develop the best therapies for the right person, at the right time.
Biomarkers play a key role in personalized medicine, also known as precision medicine. There are seven ways that we use biomarkers in research and healthcare: diagnostic, monitoring, pharmacodynamic or response, predictive, prognostic, susceptibility and risk, and safety.
Diagnostic biomarkers tell us if a person has a disease or disorder and if it is a subtype of that condition. For instance, doctors commonly use the tissue transglutaminase IgA antibody blood test for celiac disease. Another is the non-invasive fecal calprotectin test for Crohn’s disease and ulcerative colitis. This biomarker can help differentiate inflammatory bowel diseases from irritable bowel syndrome, which is a functional disorder with a few symptoms in common but completely different origins. Higher levels of calprotectin in the stool indicate IBD, whereas a lab test showing low to normal levels likely points to IBS, or IBD that is under control. Also, there are molecular biomarkers in your blood that can differentiate diarrhea predominant irritable bowel syndrome, from IBD.
Monitoring biomarkers show how a disease develops and responds to treatment. Fever is a simple but valuable biomarker of infection. Recording your blood pressure is a physiologic type of a monitoring biomarker. Another example is the carcinoembryonic antigen test to identify colorectal cancer recurrence in some patients. For pancreatic cancer, a blood test that measures the cancer antigen 19-9 can help monitor the size of the tumour and effectiveness of treatments in some patients, as well as its recurrence. Physicians can also use this test to monitor other cancers, such as colon cancer and stomach cancer.
For Crohn’s disease, there are protein-based biomarkers that can detect remission. Currently, the gold standard for identifying remission is endoscopy so the validation and use of these biomarkers might provide a more accessible and non-invasive option for patients in the future.
Pharmacodynamic or response biomarkers indicate whether you responded to a drug or therapy, such as a change in your heart rate. Response biomarkers can help physicians with dosing recommendations for a drug, how long a person should be on this medication, and more. Inflammatory response biomarkers can help identify the most effective treatment options for esophageal cancer.
Predictive biomarkers can identify whether you are at risk to develop a particular disease and how you will respond to a specific treatment. These can provide your physician with guidance as to the most appropriate treatment for a subtype of a disease or disorder. For example, the BRCA mutated proteins are potential predictive biomarkers for pancreatic cancer.
If you received a diagnosis for a health condition, prognostic biomarkers could provide information on its potential to progress or come back again, or if you are at risk for a particular health outcome. For people with active IBD, a blood-based biomarker can tell if you might have aggressive disease and need prompt treatment escalation.
Susceptibility and risk biomarkers evaluate the level of risk you have for a disease or disorder before you receive a diagnosis. H. pylori infection biomarkers are associated with an increased risk for stomach cancer.
Safety biomarkers measure the possibility of a toxic or adverse reaction that can develop from treatment. Increased levels of aminotransferases and bilirubin, a yellow pigment product, are safety biomarkers that predict serious liver damage.
Biomarkers are complex. Challenges remain with the accessibility, education, and affordability of testing across Canada. Fortunately, research continues to grow, especially on how we can use biological markers to develop the right treatment for the right person, at the right time.