Fecal Microbiota Transplant
For Severe C. diff Infections
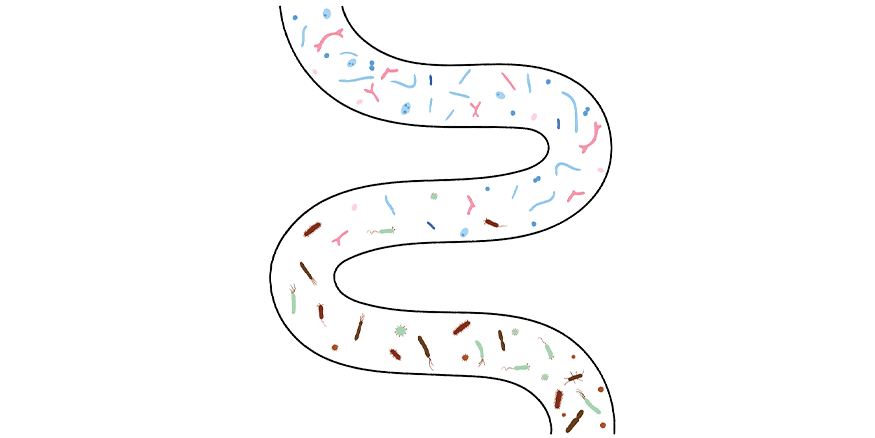
Our digestive tract can contain as many as 1,000 different species of microorganisms living in harmonious balance, most of which are harmless or even helpful. However, disrupting this balance can lead to illness. This is particularly the case with certain microorganisms, such as the Clostridioides difficile (C. diff) bacterium, formerly known as Clostridium difficile. Some of us have a small amount of C. diff bacteria in our digestive tracts without any ill effects, but it can grow out of control and lead to Clostridioides difficile infection (CDI).
Infection with C. diff is the most common cause of infectious diarrhea in hospitals and long-term care facilities. Patients often develop the infection while receiving treatment for another ailment or from touching infected surfaces in high-traffic healthcare settings. This is because the C. diff bacterium and its spores occur in high amounts in the feces of infected people who can spread the infection to surfaces if they do not wash their hands properly after using the toilet, and if proper cleaning protocols are not in place.
Symptoms include intense liquid diarrhea, dehydration, fever, appetite loss, and abdominal pain and tenderness, which can often be severe and usually requires hospitalization under intensive care. In very serious cases, it can result in death.
Treatments for Clostridioides difficile infection
Currently, the standard of care for CDI is treatment with antibiotics, but C. diff is resistant to many types of antibiotics, so this treatment can be ineffective, even though there are some targeted antibiotics with better results.
In addition to painful, difficult symptoms and increasing rates of infection, the mortality from Clostridioides difficile infection is high, ranging from 30-60%. While hospitals and care homes have implemented protocols to ensure cleanliness, many are still experiencing outbreaks. With the above considerations, finding an effective treatment is unquestionably crucial.
Fecal Microbiota Transplant
A small, retrospective study from New York, published in 2019,1 reviewed hospital records to demonstrate fecal microbiota transplant (FMT) as an effective treatment for recurrent CDI. During fecal microbiota transplantation, physicians take stool from healthy individuals and liquefy it so they can insert it directly, usually via enema or colonoscopy, through the rectum into the colon of individuals who are suffering from ailments that it might help (e.g., CDI, ulcerative colitis). This allows for a full range of microbiota to re-populate the colon rather than trying to identify and isolate individual helpful bacteria.
The study authors pulled from 426 patient records, collected over a five-year period, who had severe or fulminant C. diff infection, were in intensive care, and were taking oral antibiotics. A fulminant case of CDI differs from severe in that it consists of a sudden and complicated onset of severe symptoms.2 Of these, they identified 48 records from which they created a group (32) who had received antibiotics only and another group (16) who received oral antibiotics as well as fecal microbiota transplant. They matched patient records from both groups to each other, according to factors including age, sex, medical history, and disease severity.
Researchers found that adding FMT to the standard of care resulted in a significant decrease in mortality rates (77%) compared to those who received only oral antibiotics in intensive care. Patients who received FMT also had fewer serious adverse events compared to the control group.
Outlook
This study only looked at a small number of cases, but the results were strong. The authors call for future studies to observe similar patient populations to confirm their findings and encourage awareness among healthcare professionals on the therapeutic advantages of fecal microbiota transplant for critically ill patients with Clostridioides difficile infection. Intervention should begin earlier than nine days following diagnosis, as this might further decrease mortality rates.















