
Bariatric Surgery
Obesity is a complex disease with many potential causes and influences. It occurs when you have enough excess body fat that it increases your risk for other diseases. The first line of treatment for obesity is typically lifestyle modifications, including diet and exercise. If this doesn’t work, your physician might prescribe a medication to help control your appetite. For individuals who have severe obesity, or are suffering from weight-related diseases, weight loss surgery, called bariatric surgery, is another option. It is the most effective weight loss tool but, due to its higher risk of complications, is often a last resort.
Defining Obesity
Although other methods of diagnosing obesity are emerging, the most common way is to calculate an individual’s body mass index (BMI) by dividing a person’s weight in kilograms by his or her height in metres squared (kg/m2). Medical experts define overweight as a BMI of 25-29.9 kg/m2 and obesity as a body mass index (BMI) of 30 kg/m2 or greater. There are further categorizations for increasing levels of obesity severity (see chart). As an example, an individual who is 1.73 m (5’8”) would receive a diagnosis of obesity at 90 kg (197 lbs), class II obesity at 105 kg (230 lbs), and class III obesity at 120 kg (263 lbs). In some cases, your physician might diagnose you with obesity at a lower BMI, such as if you have a higher than expected percentage of body fat for your height and weight.
Body Mass Index
Calculate your BMI by dividing your weight in kilograms by your height in metres squared and compare to the following chart or use the online calculator.
| Underweight | <18.5 |
| Normal/Ideal weight | 18.5-24.9 |
| Overweight | 25-29.9 |
| Obesity Class I | 30-34.9 |
| Obesity Class II | 35-39.9 |
| Obesity Class III | ≥40 |
How do I Qualify for Bariatric Surgery?
The higher your BMI, the more likely your physician will recommend weight-loss surgery for you. Typically, physicians advise against surgery for individuals with a BMI from 30-40 kg/m2, and only recommend surgery for those with a BMI ≥40 kg/m2 who have been unable to attain weight loss through dietary changes, exercise, and/or medications. However, surgery is sometimes best for those who have a BMI ≥35 kg/m2 along with weight-related health complications (e.g., sleep apnea, type 2 diabetes, hypertension). Physicians typically will not perform bariatric surgery on those who are 18 years or younger, persons with untreated psychiatric conditions, people who have conditions that would make it unsafe for them to undergo surgery, individuals who are not willing to commit to the lifestyle and dietary changes necessary to ensure a successful outcome after surgery, and women who are pregnant or breastfeeding, or who plan on becoming pregnant within two years of their expected surgery date.
Types of Bariatric Surgery
There are four main types of bariatric surgery currently available in Canada: gastric sleeve, Roux-en-Y gastric bypass, gastric band, and intragastric balloons. Bariatric surgery works by limiting the amount of food you can eat at once and/or reducing your body’s ability to absorb calories from the food you eat. These physical changes can also lead to hormonal changes, which can help reduce appetite and cravings.
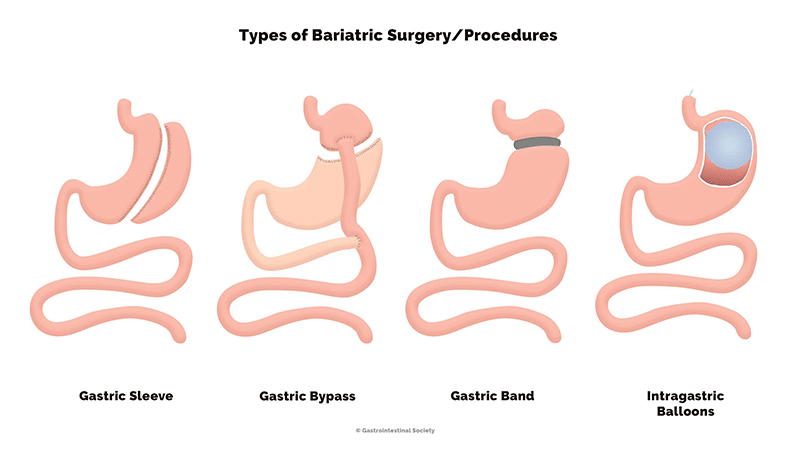
Gastric Sleeve
In this procedure, a surgeon will remove part of your stomach, leaving behind just a thin sleeve, the size of a small banana. The surgeon will perform this surgery laparoscopically, which is a less invasive form of surgery that involves just a few small incisions. The gastric sleeve creates a smaller stomach sac, and thereby reduces the amount of food you can eat during a window of time. When you eat, your stomach becomes full quickly, so it sends signals to your brain indicating that you have eaten enough much sooner than it normally would. In addition, since your stomach produces the hormone ghrelin, which stimulates hunger, removing some of the tissue that creates the hormone means that your body will produce less of it.
Gastric Bypass
In a gastric bypass, also known as a Roux-en-Y gastric bypass, the surgeon will remove part of your stomach, leaving just a small pouch, and then connect this new pouch to the middle of your small intestine. This surgery is highly effective because a smaller stomach means that you can’t eat as much, and your body won’t absorb as many calories because of the additional small intestine bypass. As in gastric sleeve surgery, a gastric bypass also affects hormonal production and regulation in a manner that reduces appetite and makes obtaining and maintaining a lower weight easier. However, there are greater risks with gastric bypass than the other forms of bariatric surgery, since it is remodeling several sections of the digestive tract and is therefore a more complex procedure. But, for many individuals, the surgery is worth the increased risk because it has a remarkably high success rate.
Gastric Band
This technique involves a surgeon placing a band around the upper part of the stomach to create a smaller pouch. The surgeon will perform the surgery laparoscopically and can adjust the band by injecting saline into it to make the available stomach area smaller or larger, as needed. However, since there is a foreign object in your body, several unique complications can occur. The band can slip out of place, tear open and leak, wear away at the stomach, and cause blockages.1
Intragastric Balloons:2
This is a temporary measure that involves placing a fluid-filled balloon into the stomach. It works by helping you feel full sooner and delaying the rate of gastric emptying, so that you feel full longer. It is different from other methods of surgery as it does not involve modifying the structure of the digestive tract and it is reversible, but it still has risks. These include pancreatitis, balloon over-inflation, or developing a hole/tear (perforation) in the stomach or esophagus.3 If the balloon deflates, it could move through your digestive tract and cause a blockage, which could potentially require surgery to remove. Due to the temporary nature of this procedure, and it being a newer offering, there is less data on its long-term effectiveness.
Preparing for Bariatric Surgery
Before your surgery, it is important to try to maintain good health. Now is a good time to quit smoking, as it can reduce your body’s ability to heal after surgery, and it is best to cut down on alcohol as well. After your surgery, you will need to make drastic changes to the way you eat, so it is helpful to ease into these changes beforehand. This means eating smaller, more nutrient-dense meals and getting a moderate amount of low-impact exercise. Your physician will likely tell you to follow a strict diet in the weeks leading up to your surgery, in order to start your weight loss and reduce the amount of fat in your liver. These changes will contribute to a more successful surgical outcome. Closer to your surgery date, you will need to go on a liquid diet, usually consisting primarily of protein shakes. Make sure to follow all the instructions your healthcare team provides.
Recovering from Bariatric Surgery
Recovery will depend on the type of surgery you have. Typically, you will need to follow a liquid diet, sip on water throughout the day, and avoid strenuous activities for a few weeks to allow your body to heal. Once you are able to eat solid foods, you will still be eating differently than you did before you had your surgery. Your portions will be much smaller, so it is important to ensure that the foods you eat are nutritious. Bariatric surgery requires lifelong maintenance efforts to be effective. Your healthcare team will provide you with details on how to make sure you get enough nutrients, including vitamins, minerals, and protein, so you maintain good health during your recovery.
As you will be recovering from surgery and adjusting to a smaller stomach and/or reduced small intestine length, many symptoms are normal, including nausea, constipation, pain and soreness, and swelling, bruising, and itching around the incision.
However, make sure you attend all follow up appointments with your physician and seek medical care immediately if you notice any concerning symptoms after your surgery, including fever, unusual swelling or discharge from your wound, excessive nausea or vomiting, the inability to urinate, chest pain, or shortness of breath.
Another thing to consider is that some individuals say they do not get enough support from their healthcare team after bariatric surgery. It can be helpful to look into support groups or ask your doctor for information on any available support programs to help ensure a successful outcome.
Benefits of Bariatric Surgery
Overall, bariatric surgery performed in Canada is safe, and the mortality rate is less than 1%.4 While there are risks, the outcome is usually more positive than negative. Successful bariatric surgery often results in significant, long-term weight loss, and there is good evidence that bariatric surgery can improve or reverse type 2 diabetes, hypertension, sleep apnea, osteoarthritis, and hormonal imbalances.5
Bariatric surgery is much more effective than other methods of weight loss. For many individuals who struggle for decades with diet, exercise, and medications that are ineffective, surgery is often the method that finally gives them lasting weight loss. Studies have shown remarkable results after five years, with a total loss of excess weight of 93% in those who had gastric bypass surgery, 60% in gastric sleeve surgery, and 59% in gastric band surgery.6,7
Typically, individuals who try to lose weight by eating less find it exceedingly difficult to stick with, as maintaining a constant caloric deficit is not sustainable for most people. Since weight-loss surgery reduces the amount of food you can eat physically, and in some types of surgery can modify the levels of hormones responsible for hunger or reduce the calories your body absorbs, it is generally effective at regulating appetite, so it is easier to stick to your diet plan.
Negative Effects of Bariatric Surgery
While most people experience relatively few side effects, in comparison to the overall positive benefit, there are still some potential complications. For example, nausea and constipation are common. However, several more severe complications can occur, including ulcers, gallstones, small bowel obstruction, and dumping syndrome.6 There is also some evidence of potentially severe nutritional, and pharmacological consequences of bariatric surgery. Iron deficiency anemia after bariatric procedures can result from intestinal bleeding (e.g., from marginal ulcers) or reduced iron absorption due to postoperative intolerance for red meat, diminished gastric acid secretion, or exclusion/removal of the duodenum. In a large, patient record review of 959 patients who underwent laparoscopic Roux-en-Y gastric bypass between 2001 and 2011,8 51% were iron deficient and 7% required intravenous iron therapy. Comparing different types of surgery, a cross-sectional pilot study of 95 patients showed no significant difference in iron deficiency rates after Roux-en-Y gastric bypass or sleeve gastrectomy (30% vs 36%).9
Conclusion
Remember that while bariatric surgery is effective, it will not lead to instant weight loss. You still have to focus on any underlying causes of obesity and making changes to your diet and exercise routine that will last for the rest of your life. However, with proper management, bariatric surgery can lead to successful weight loss and reverse or prevent obesity-related diseases and disorders.
Want to learn more about obesity?
We have several related articles that may be helpful:
- Obesity
- Obesity Video
- Obesity Journey Video
- Obesity Journey Survey Report 2024
- Obesity Survey Results 2021
- Obesity Medications
- Bariatric Surgery
- Hunger and Appetite
- GI Issues Associated with Obesity
- Marty Enokson’s Battle with Obesity
- Don’t Blame the Patient
