Click here to download a PDF of this information.
Inflammatory Bowel Disease
Intestinal Anatomy
 To understand IBD, a review of gastrointestinal (GI) tract anatomy is helpful. This explanation is not complete, but it covers the basics.
To understand IBD, a review of gastrointestinal (GI) tract anatomy is helpful. This explanation is not complete, but it covers the basics.
The digestive system consists of a long tube (alimentary canal) that varies in shape and purpose as it winds its way through the body from the mouth to the anus (see diagram). The size and shape of the digestive tract varies according to the individual (e.g., age, sex, size, and disease state). The dimensions mentioned below are for an average adult male.
The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. In the mouth, chewing mechanically breaks down and mixes food, while saliva begins to modify it chemically, thus beginning the digestive process. Chewing and swallowing (ingesting) require conscious effort, but once food reaches the esophagus, an automatic, rhythmic motion (peristalsis) takes over, propelling the contents along. Several body systems provide the chemicals necessary to complete digestion, absorption, and elimination. If all is going well, the passage of food from one area of the intestines to the next is precisely coordinated, so that it stays in each area for just the right amount of time.
Transit time is the duration between when you take a bite of your meal and when leftover waste finally passes out as stool (feces). A meal could take anywhere from 12-72 hours to travel through the digestive tract. Each person is unique; a normal bowel movement pattern for one person may be very different from those of family members or friends. Some individuals have an irregular pattern, never knowing what to expect. The composition and quantity of dietary intake, the presence of a GI disease or disorder, and other factors influence transit time.
Following the esophagus, located within the left side of the abdominal cavity, is the stomach, a sac-like organ about 25 cm (~10″) long. It increases in diameter as it receives food, holding up to a maximum of about 4 litres (but do not eat so much as to extend the stomach fully). Strong chemicals break food down into smaller components, while the stomach’s thick walls keep these chemicals from entering the body as it squeezes its contents with strong circular and longitudinal muscles.
The lower part of the GI tract includes the small and large intestines. The names of these parts are a bit confusing, as the small intestine is about three times as long as the large intestine. Small and large refer to the diameter, which for the small intestine is about 2.5-3 cm (~1″) compared to 6.5-7 cm (~2.5″) for the large intestine.
The small intestine is a long and narrow coiled tube that extends from the stomach to the large intestine, winding around within the abdomen. It has an enormous internal surface area due to the presence of millions of tiny finger-like protrusions called villi, which are covered in hair-like protrusions called microvilli. This is where most digestion and absorption of food takes place. The first section of the small intestine, the duodenum, is the smallest segment, which is about the same length as the stomach (25 cm/~10″), followed by the jejunum (2.5 m/~8′) and the ileum (3.5 m/~11.5′), for a combined total of a little more than 6 m (~20′). Functions of the small intestine include secreting digestive enzymes and buffers, and absorbing nutrients. Iron is absorbed in the duodenum, and vitamin B12 and bile salts are absorbed in the last part of the ileum (terminal ileum).
The mucosa is the innermost layer of the GI tract wall. In the small intestine, it is responsible for both the secretion of digestive juices and the absorption of nutrients. The second layer is the submucosa, which consists of a dense layer of connective tissue with blood vessels, lymphatic vessels, and nerves. Outside of the submucosa is a layer of muscle, the muscularis externa. As these muscles contract, they propel food along the digestive tract. The outermost layer is the serosa, a thin layer of cells that secrete fluid, which reduces the friction caused by muscle movement.
The first part of the colon, the cecum, connects to the small intestine at the ileocecal valve, in the lower right area of the abdomen. The rest of the large bowel consists of the ascending colon (going upward on the right side of the abdomen), transverse colon (going leftward across the abdomen), and descending colon (going downward on the left side of the body), followed by the sigmoid colon. Altogether, the large intestine (colon) is about 1.25 m (~4′) long. The main function of the colon is to absorb water, form stool, and eliminate waste. The large intestine does not secrete digestive enzymes and does not have villi. The colon contains many varieties of friendly bacteria and yeasts to aid digestion and to prevent proliferation of harmful bacteria and yeasts. The colon ends in the rectum (about 15-20 cm/~6-8″ long), which briefly stores waste material until it is eliminated via the anus as stool, usually as a conscious choice.
Although not directly part of the digestive tract, the liver, gallbladder, and pancreas serve as accessory organs that are vital to the digestive process.
Watch and Share This IBD Q&A Video!
Inflammatory Bowel Disease
Since we are all unique, issues discussed here will not apply to every person with IBD. However, we hope this information helps you understand this complex and chronic disease. Please be sure to discuss your particular circumstances with the healthcare professionals involved in your care.
Inflammatory bowel disease is a term that primarily refers to two diseases of the intestines: Crohn’s disease and ulcerative colitis. These diseases have a few similarities but differ significantly in two key ways: the area of the digestive tract affected and the extent of the inflammation.
Area Affected: Ulcerative colitis only involves the colon and always begins at the anus, with the disease continuously progressing upward. In some cases, it can involve the entire large intestine. In ulcerative proctitis, a milder form of ulcerative colitis, inflammation reaches up from the anus no more than about 20 cm (~8″). In Crohn’s disease, the inflammation can be in multiple patches or one large patch, and may involve any area throughout the entire digestive tract, often affecting the last part of the small intestine (terminal ileum).
Extent of Inflammation: In ulcerative colitis, inflammation only involves the inner mucosa, while in Crohn’s disease, inflammation can extend right through the entire thickness of the bowel wall, from the mucosa, through the muscle, and can even include the thin outermost layer of digestive tract cells (serosa).
The inflammatory process causes dilation of blood vessels with increased warmth, oozing of fluid into the tissue, infiltration with inflammatory cells, and ulceration of the mucosa.
Inflammation can result from infectious agents such as bacteria, fungi, parasites, or even viruses. It can also arise from a chemical exposure, burn, trauma, or several other causes. The exact mechanism of IBD is undetermined but there is considerable research evidence to suggest that interactions between environmental factors, intestinal bacteria, immune dysregulation, and genetic predisposition are responsible. There is an increased risk for those who have a family member with the condition.
Although Crohn’s disease is currently the proper name for the condition, sometimes you might hear older terms, such as regional enteritis, terminal ileitis, granulomatous colitis, or ileocolitis used interchangeably.
A diagnosis of inflammatory bowel disease can occur at any point throughout life, with a high occurrence in youth and then again around 40-50 years of age. Approximately 0.8% of the Canadian population has IBD. Canada has among the highest prevalence and incidence reported in the world, at approximately 322,600 individuals, with slightly more having Crohn’s disease than ulcerative colitis.
Living With IBD Videos
Symptoms of Inflammatory Bowel Disease
The most common symptom of IBD is diarrhea. Inflammation can affect transit time, usually causing food to pass more quickly and allowing less time for water absorption, resulting in watery stool. Crohn’s disease can affect the small intestine and, in doing so, it may prevent the proper absorption of food, also resulting in diarrhea and the increased elimination of fat (steatorrhea) and other nutrients. In ulcerative colitis and Crohn’s disease of the colon, the normal colon function of removing fluid from its contents is impaired, resulting in frequent, liquid stools. Since the lining of the colon may be ulcerated, the diarrhea often contains blood. In the later stages of the disease, the colon can narrow and shorten, impairing water absorption further, leading to urgency of bowel movements and poor control of elimination function. Constipation can also develop, as the body struggles to maintain normal bowel function.
Abdominal pain is another common symptom. Like muscles elsewhere in the body, the muscular coat of the intestine can spasm and inflamed intestines are irritable and more likely to spasm. This, in turn, applies pressure upon the extensive nerve endings in the bowel wall. This explains some types of pain in IBD, particularly cramping. In Crohn’s disease, pressure can build up behind a narrowed portion (stricture) of the intestine and produce pain. Occasionally, the narrowing is so severe that a blockage of the intestine occurs, requiring immediate medication and, less frequently, surgical intervention.
Fever frequently accompanies inflammation of any type and is present in IBD.
Those with IBD can experience tenesmus, which is the feeling of incomplete defecation, as well as a sudden, short, severe type of pain at the opening of the rectum.
Weight loss is common in Crohn’s disease, due to the small intestine’s decreased ability to absorb sufficient nutrition. In children, a delay in growth and maturity might result. If possible, it is best to consult a pediatric gastroenterologist, who has specific training to manage the special needs of the growing child.
In Crohn’s disease, the rectum and anus can become a focal point for inflammation, with the formation of painful inflamed slits in the skin and superficial tissues, called anal fissures. Large pus pockets or abscesses may accumulate, producing severe pain and fever. An abnormal, tunnel-like connection between the intestine and the skin, called a fistula, may occur. When this connection is near the opening of the rectum, it is called an anal fistula. Fistulae also may occur between loops of intestine within the abdomen or between the intestine and the abdominal wall. Abdominal surgery can increase the risk of fistulae.
Anemia, or low red blood cell count, commonly occurs from blood loss due to the ulcerations in the lining of the intestine. Occasionally, blood loss may be so severe that the patient requires a blood transfusion. Anemia may also be a consequence of general malnutrition due to nutrient malabsorption and the debilitating effects of IBD on a person’s body.
Other manifestations of IBD include arthritis, skin problems, liver disease, kidney stones, and eye inflammation.
If you have had ulcerative colitis or Crohn’s disease in the colon for about 10-15 years, you are at a slightly increased risk for colorectal cancer, so your physician might recommend screening for this sooner than typical for the general population.
Diagnosing Inflammatory Bowel Disease
Malfunction of the intestinal tract may occur for a wide variety of reasons and some symptoms (diarrhea, pain, and weight loss) may be very similar to symptoms of other diseases or disorders. The accurate diagnosis of IBD is essential, and a physician will take steps to exclude other conditions.
A careful evaluation of the history of the illness is the first step toward a correct diagnosis. The physician will review factors such as when and how the symptoms began, what subsequent problems occurred, the nature of the diarrhea, the type of abdominal pain, as well as the characteristics and quantity of rectal bleeding.
In ulcerative colitis, the most useful diagnostic tool is the sigmoidoscope, a short instrument that allows visualization of the inside of the lower bowel. If necessary, during this procedure a physician can biopsy any suspected areas for further investigation. Viewing the lining of the colon with this instrument at regular intervals throughout the healing process allows a physician to monitor the disease. If needed, a longer, flexible instrument called a colonoscope can help the physician see farther up into the colon, sometimes as far as the terminal ileum (where the small and large intestine meet), which is a likely location for the formation of Crohn’s disease. In some cases, a gastroscope, entering the body via the mouth, is useful to confirm Crohn’s disease in the upper part of the GI tract.
Although less likely, a physician might request a barium X-ray. When needed for the upper GI area, you will drink a liquid that coats the walls of the esophagus and stomach. This drink contains barium, which shows up as bright white on X-rays, providing a contrasting picture of the shape and function of the upper GI tract. When needed to provide details of the lower GI tract, you will undergo a barium-containing enema to allow the physician to view the contours of the bowel. However, a colonoscopy offers a diagnostic advantage over a barium enema X-ray in that a physician can take biopsies during this procedure.
Other diagnostic tools include blood tests and examination of a stool sample for infectious agents and hidden (occult) blood. Ultrasound, CT scans, and MRI are helpful in looking for complications of IBD but are not necessarily useful in making the primary diagnosis.
IBD Patient Journeys
Management of Inflammatory Bowel Disease
The treatment of inflammatory bowel disease is multi-faceted; it includes managing the symptoms and consequences of the disease along with following a medicine regimen targeted at reducing the underlying inflammation.
Dietary and Lifestyle Modifications
An important, overarching challenge is managing nutrition intake when disease has compromised the digestive system. Crohn’s disease can interfere with nutrient absorption, increasing the risk for deficiencies, but individuals with ulcerative colitis are generally at low risk, as colitis does not affect the small intestine where most nutrients are absorbed. However, there are other factors and symptoms contributing to malnutrition in patients with either disease.
Depending on disease symptoms, a person with IBD may feel unwell, and the sensations of food passing through the digestive tract can be so uncomfortable that this might lead to food avoidance or food choices that might not provide a balanced diet. Better overall nutrition offers the body a better base from which to heal itself, but dietary changes on their own are insufficient to address inflammatory bowel diseases.
If bleeding is excessive, anemia may occur, and further modifications to the diet will be necessary to compensate for this.
Depending on the extent and location of inflammation, you might have to follow a special diet, including supplementation. It is important to follow Canada’s Food Guide, but this is not easy for individuals with IBD. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate and increase symptoms even though they do not worsen the disease.
Particularly in Crohn’s disease during symptom flare-up, and sometimes in ulcerative colitis, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes (elemental formulations), and fasting with intravenous feeding (total parenteral nutrition) can achieve incremental degrees of bowel rest.
Symptomatic Medication Therapy
The symptoms of IBD are the most distressing component of the disease, and direct treatment of these symptoms, particularly pain and diarrhea, will improve quality of life. A number of treatments exist to address diarrhea and pain. Dietary adjustment may be beneficial and anti-diarrheal medications have a major role to play. Analgesics can be helpful for managing pain not controlled by drugs that address the underlying inflammation, listed below. Acetaminophen (Tylenol®) is preferred over medications called non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen (Advil®, Motrin®), and naproxen (Aleve®, Naprosyn®), as they can irritate the gut.
There are two types of anti-diarrheal medications directed at preventing cramps and controlling defecation. One group alters the muscle activity of the intestine, slowing down content transit. These include: non-narcotic loperamide (Imodium®); narcotic agents diphenoxylate (Lomotil®), codeine, opium tincture and paregoric (camphor/opium); and anti-spasmodic agents dicyclomine HCL and hyoscine butylbromide (Buscopan®).
The other group adjusts stool looseness and frequency by soaking up (binding to) water, regulating stool consistency so it is of a form that is easy to pass. Plant-based products are helpful such as inulin fibre (Benefibre®) and psyllium (ispaghula) husk (Metamucil®). Plant fibres are also useful to manage constipation, due to their stool regulating effects. Cholestyramine resin, a bile salt binder, can also help with stool looseness.
If extra-intestinal signs of IBD occur, such as arthritis or inflamed eyes, your physician will address these conditions individually, as you might require referrals to other specialists. If anxiety and stress are major factors, a program of stress management may be valuable.
Individuals with IBD may be anemic from a combination of factors, such as chronic blood loss or malabsorption of certain vitamins and minerals. Iron supplements could help improve this condition, with oral heme iron polypeptide (e.g., Hemaforte 1, Hemeboost, OptiFer® Alpha, Proferrin®) being the preferred option, due to quick-acting and low side-effect profiles. Iron isomaltoside 1000 (Monoferric™), iron sucrose (Venofer®), and sodium ferric gluconate (Ferrlecit®) are indicated for intravenous (IV) treatment of iron deficiency anemia in adults who have intolerance or unresponsiveness to oral iron therapy. Occasionally, a blood transfusion may be necessary.
The most widely prescribed antibiotics are ciprofloxacin (Cipro®) and metronidazole (Flagyl®). Broad-spectrum antibiotics are important in treating secondary manifestations of the disease, such as peri-anal abscess and fistulae.
Anti-Inflammatory Medication Therapy
There are two goals of treatment for IBD: induction of remission, which is marked by the absence of symptoms and inflammation in the affected part of the gastrointestinal tract, followed by maintenance of remission (prevention of flare-ups).
To accomplish these goals, physicians aim treatment at controlling the ongoing inflammation in the intestinal tract, which will lead to improved symptoms. Treatments come in many forms, using various body systems. A physician may prescribe any of the following medications alone or in combination. It could take some time to find the right mix for an individual, as each case of IBD is unique. Depending on the location of your disease, a combination of drug delivery methods (oral and rectal) could help to ensure that all areas of the disease are covered.
5-Aminosalicylic Acid (5-ASA)
The medication used to reduce inflammation in mild to moderate IBD with the longest record of success worldwide is 5-ASA, including mesalamine (Mezavant®, Mezera®, Octasa®, Pentasa®, Salofalk®) and olsalazine sodium (Dipentum®), available orally in tablet and capsule forms. 5-ASA medication is generally safe and well tolerated for long-term use. Depending on the location of your disease, you may be required to administer mesalamine (Pentasa®, Salofalk®) rectally, in the forms of enemas or suppositories. Mezera® is available as a foam enema. Octasa® is available as an oral tablet, taken once daily, for individuals living with ulcerative colitis. Patients typically use rectal medications nightly at first and, as the disease improves, treatments can become less frequent.
5-ASA helps to settle acute inflammation and, when taken on a long-term basis (maintenance), it tends to keep the inflammation inactive. It is important to keep up your medicine regimen even if your symptoms disappear and you feel well again. Maintenance therapy can be at the full initial dosage or at a reduced dosage and interval, depending on the disease response.
A combination of 5-ASA and sulfa antibiotic is available orally as sulfasalazine (Salazopyrin®).
Corticosteroids
To reduce inflammation for a shorter-term, corticosteroids might help. Oral medications include prednisone for mild to severe IBD and budesonide (Cortiment® for ulcerative colitis; Entocort® for Crohn’s disease) for mild to moderate disease, although prednisone tends to have greater side effects. Oral budesonide (Cortiment®, Entocort®) comes in two brands, which release medication at different points in the digestive tract. Hydrocortisone and betamethasone are available in rectal formulations (enemas, foams, and suppositories). A new rectal foam, budesonide (Uceris®), and an oral medication for hydrocortisone (Auro-Hydrocortisone), are also available for use in ulcerative colitis.
Physicians might prescribe hydrocortisone (Solu-Cortef®) and methylprednisolone (Solu-Medrol®) for administration intravenously in-hospital. Corticosteroids should not be used for longer-term or maintenance therapy.
Oral vs. Rectal 5-ASAs or Corticosteroids
Most physicians prescribe oral versions of 5-ASAs or corticosteroids, as this is a patient-preferred medication delivery method. However, even if these medicines have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool – and the fact that IBD often causes diarrhea – might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by delivering the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema (liquid form) will reach farther, about 60 cm. Patients usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not usually interfere with the drug, as the rectal area is typically relatively empty right before bed.
Rectal preparations are particularly good at treating urgency and bleeding, which are bothersome symptoms. A positive response often occurs within days of treatment.
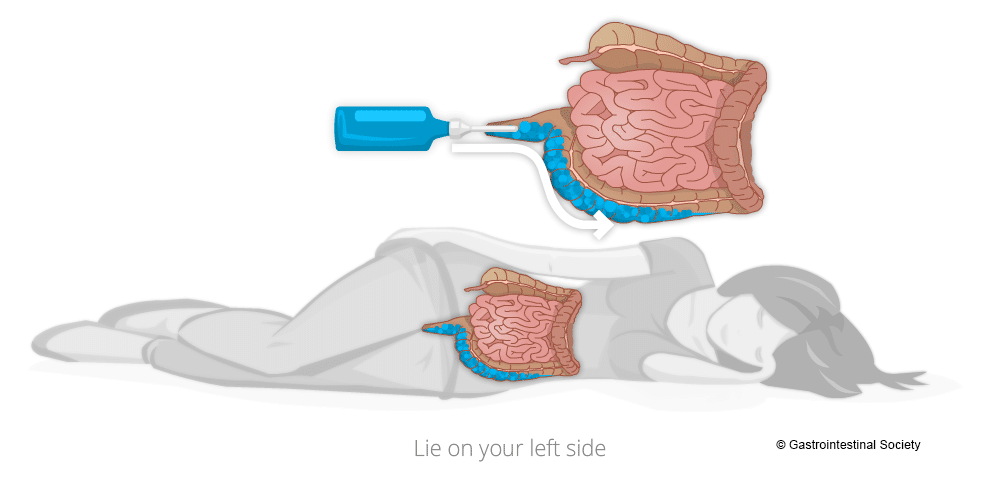
Administering Rectal Therapies
To get the best coverage of topical rectal therapies, it is best to lie down on your left side. As you will see from the accompanying diagrams, the human anatomy is not symmetrical and the way the organs lay when on the left side makes for better medication administration. Talk with your pharmacist for more information to help with proper use and administration of rectal therapies.
Immunosuppressive Agents
Small Molecules
Physicians prescribe these drugs to prevent flare-ups of IBD, and to try to reduce dependence on steroids. They include azathioprine (Imuran®), cyclosporine, mercaptopurine/6-MP (Purinethol®), and methotrexate sodium (Metoject®). These medications can take up to twelve weeks of therapy to start working and six months to be fully effective.
There are newer classes of medications that target inflammation. These are Janus kinase (JAK) inhibitors and sphingosine-1-phosphate (S1P) inhibitors. JAK inhibitors typically work faster than biologics, pose no risk for immunogenicity, and are easy and convenient to take since they are in pill form. These include a pan-JAK-inhibitor tofacitinib (Xeljanz® for ulcerative colitis) and a selective JAK-inhibitor upadacitinib (Rinvoq® for Crohn’s disease and ulcerative colitis).
S1P inhibitors are immunomodulators and act as a receptor agonist, sequestering lymphocytes to peripheral lymphoid organs and away from their sites of chronic inflammation. These include ozaminod (Zeposia®) and etrasimod (Velsipity™), which are currently only available for individuals with ulcerative colitis.
Biologics (Large Molecules)
Biologic medications are important treatment options for those who have moderate to severe IBD. These products are specifically developed proteins that selectively block molecules involved in the inflammatory process. Gastroenterologists routinely prescribe biologics to reduce inflammation and control the symptoms (induce clinical remission) of IBD.
The first biologic that Health Canada approved to treat Crohn’s disease was the anti-TNF agent infliximab (Remicade®) in 2001 (2006 for ulcerative colitis). Later biologics include anti-TNF agents, adalimumab (Humira®) and golimumab (Simponi® for ulcerative colitis), an alpha-4/beta-7 integrin inhibitor, vedolizumab (Entyvio®), an IL-12/23 inhibitor, ustekinumab (Stelara®), and IL-23 inhibitors, risankizumab (Skyrizi® for Crohn’s disease) and mirikizumab (Omvoh™ for ulcerative colitis). As the patents expire for these medications, their biosimilars come to market. So far, there are biosimilars of infliximab (Avsola®, Inflectra®, Ixifi®, Omvyence™, Remsima™SC, Renflexis®), adalimumab (Abrilada®, Amgevita®, Hadlima®, Hadlima® PushTouch®, Hulio®, Hyrimoz®, Idacio®, Simlandi™, Yuflyma™), and ustekinumab (Wezlana™). See our website for more information about biosimilars.
These medications are proteins, which our bodies might identify as foreign invaders and then develop antibodies to fight them off, which can diminish the drug’s effectiveness over time. If you take a break from the medication and then try to resume it, what worked wonderfully for you before might not work the next time you take it because of these antibodies. This means that it is extremely important that you only stop treatment if your physician advises you to do so. Stopping a treatment because you are feeling well might result in that drug not working to make you feel well again in the future.
Humira® (and its biosimilars), Entyvio®, Simponi®, Stelara® (and its biosimilar), Skyrizi®, and Omvoh™ are available for self-administration under the skin (subcutaneous). Remicade® (and its biosimilars, except Remsima™SC), Entyvio®, Stelara®IV, and Wezlana™IV are available as intravenous (IV) infusion by a healthcare professional. The dosage of both types can be in various intervals, depending on the medication and the response. In some cases, you might need to start on a biologic medication by receiving it as an IV infusion and then move on to subcutaneous injection for maintenance.
One tool to help physicians be sure that patients are on the right medication at the right dose is Therapeutic Drug Monitoring (TDM), which involves laboratory testing to determine the level of the drug in the system. A second vital test is fecal calprotectin, which measures an inflammatory substance in your stool. A gastroenterologist assesses these results in the context of a person’s symptoms at specific periods during the treatment schedule.
Surgery
In those who have ongoing active disease that fails to respond to all forms of medical management, surgery might be necessary. Since inflammatory bowel diseases are systemic, not only the bowel is involved. Therefore, removing diseased tissue, although sometimes necessary, does not remove the disease.
Ulcerative colitis only involves the large intestine, so removing this organ will remove the disease from the digestive tract, but it is not a cure. Removing the colon can lead to other symptoms and complications. Although there are many variations to possible surgical procedures, a surgeon typically removes all or part of the colon (colectomy) and then brings the end of the remaining intestine through a new surgical opening in the abdominal wall (ostomy) to which the patient can attach a removable appliance to collect stool. An ostomy may be either temporary or permanent, depending upon the particular situation.
Newer techniques have arisen whereby surgeons can preserve the anal muscle and create an internal pouch, or reservoir, from the remaining intestine so that emptying pouch contents via the anus more closely resembles the normal anatomical route. However, with the loss of colon function, bowel movements have very high liquid content and move very frequently. This means that even after surgery, patients could face troublesome gastrointestinal symptoms. One complication that can occur is pouchitis, which is inflammation within the surgically created pouch.
Crohn’s disease tends to recur, in as many as 75% of patients, even after surgical removal of all visible and microscopic disease in the digestive tract. Inflammation can recur months or years later and can be present elsewhere in the body. Physicians reserve surgery as only a last alternative, usually in cases when medical management fails, or for complications such as obstruction, fistulae, or abscess formation.
An emerging surgical therapy is intestinal transplantation, but there are barriers yet to overcome, such as tissue rejection and inflammation in the newly transplanted organ.
What is a Flare?
When you have inflammatory bowel disease, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms aren’t present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes to treat your IBD, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs (including aspirin, ibuprofen, and naproxen) can also make you more susceptible to a flare.
IBD Flare Video
When to Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with IBD, but it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Flare Treatment Options
It is important to discuss with your physician in advance exactly what they would like you to do if the disease flares, particularly if you are seeing a gastroenterologist who has a long waiting time to get an appointment. You might be taking medication regularly but still experience a flare. Typically, your physician will provide a prescription for a rectal preparation that you could purchase and use immediately, to avoid going untreated while waiting to get into the office. However, your physician might still want you to call the office to report your symptoms. This is an important conversation to have with your healthcare team, so you can prepare for self-management, when necessary, while keeping them aware of your condition.
When you are having disease symptoms, the first step is usually to increase (step up) your current treatment. Ask your doctor to explain your options as to what you should do between visits:
- increase the dose of your oral medication (tablets)
- use a rectal formulation (suppository or enema)
- a combination of the above
Your specific situation and history will determine what your physician recommends. Ideally, you should have a plan in place outlining what you can do if you have a flare. However, if you have severe symptoms you should seek immediate help, even if that means heading to the hospital emergency room.
Is it important to treat a flare early, or is it ok to wait a bit?
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline (5-ASA) treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing a worsening of your symptoms, you probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual (during colonoscopy) evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Looking into the colon gives a better, more reliable picture of what is truly going on with your disease. For this reason, your specialist might suggest a colonoscopy so he or she can have a closer look inside your colon to determine the best course of action. However, in most instances, a physician might still base a decision to prescribe medication on the severity and the nature of your symptoms. This is particularly the case when the symptoms are still mild.
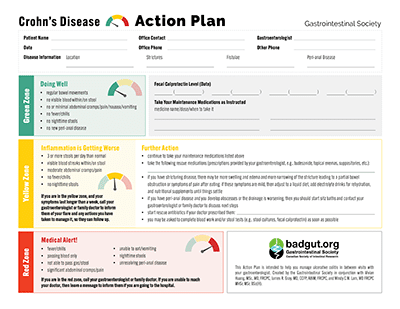
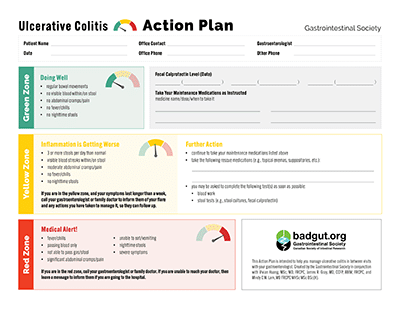
Action Plans
Want to learn more about managing flares? We have printable Action Plans available for both Crohn’s disease and ulcerative colitis. These documents outline which symptoms are normal, which indicate a flare, and which require emergency care. They also contain spaces to write in details about your medications, disease status, and healthcare team contact information.
Other Types of IBD
While most cases of IBD are either Crohn’s disease or ulcerative colitis, these aren’t the only types of IBD. The following are rare types of IBD, some of which it is possible to recover from completely.
Ischemic Colitis
The word ‘ischemia’ refers to an inadequate blood flow to a certain part of the body. This lack of blood supply means that not enough oxygen, glucose, and other materials are able to reach the cells to keep them alive and functioning. Ischemic colitis is the disease that occurs when reduced blood flow to the digestive tract causes inflammation and injury, which leads to IBD symptoms. Ischemic colitis typically occurs in the left area of the abdomen, where it causes considerable pain.
The reduced blood flow can come from a problem with the body’s circulation, such as low blood pressure, or localized events that cause reduced blood flow around the intestinal tract, including blood clots and narrowed or blocked blood vessels. However, there is often no identifiable cause.
Treatment often involves intravenous nutrition to allow the bowel to rest, which typically resolves the disease within one or two weeks. However, in some cases, surgery might be necessary.
Diversion Colitis
There are many reasons that a person might require an ileostomy or a colostomy, and these include intestinal obstruction, bowel injury, infection in the bowel, and colorectal cancer. Some individuals with ulcerative colitis or Crohn’s disease require an ostomy after having damaged tissue removed. There are many risks to this type of surgery, one of which is diversion colitis. Diversion colitis often disappears after full healing from the ostomy surgery, but sometimes further anti-inflammatory treatment is necessary.
Radiation Enteritis
This disease occurs as a complication from radiation therapy, during which radiation of the abdominal area causes irritation and inflammation to the intestine. Physicians take precautions to avoid radiation exposure to the intestine, but sometimes damage does occur. Many individuals undergoing radiation develop acute radiation enteritis, which is temporary, but some patients develop chronic radiation enteritis, which can last for months or years after radiation treatment. Symptoms include diarrhea, abdominal pain and cramping, rectal bleeding, and nausea. Treatment involves dietary changes to increase nutrient intake and to allow the bowel to heal, and taking medications to treat diarrhea, pain, and inflammation. If symptoms are severe, it might be necessary for the patient to cease radiation therapy, and possibly undergo surgery.
Microscopic Colitis (Lymphocytic Colitis & Collagenous Colitis)
There are two types of microscopic colitis, so called because the inflammation is too small to detect during colonoscopy, and requires microscope analysis of a tissue sample (biopsy). Microscopic colitis includes collagenous colitis and lymphocytic colitis. It is common for physicians to mistake symptoms of microscopic colitis for other conditions, such as irritable bowel syndrome, gastroenteritis, and celiac disease. The most common symptoms include abdominal pain and watery diarrhea that is not bloody. Researchers believe that in some cases, non-steroidal anti-inflammatory drugs (NSAIDs) can cause this disease, because ceasing to take these medications can result in symptom resolution.
We still don’t know much about the development, progression, and treatment of these diseases. The key differentiation between collagenous colitis and lymphocytic colitis is that collagenous colitis involves thickening of the sub-epithelial collagen table and lymphocytic colitis does not. Lymphocytic colitis affects females and males equally, but collagenous colitis is more common in women, with approximately 90% of cases affecting females, typically between 50-70 years of age.
Treatment can involve cessation of NSAIDs if the physician believes it could be the cause, and in some cases taking medications, such as 5-ASA, might be necessary.
Inflammatory Bowel Disease Outlook
The future lies in education and research. Education of both the public and the medical profession is required to emphasize the importance of inflammatory bowel disease research. Many of the following areas need further investigation:
- the chemistry of the normal, as well as diseased, intestine,
- further study of tissue changes that occur in inflammation,
- genetic factors,
- the role of nutrition,
- gut bacteria,
- the relative incidence of the diseases, as determined by accurate population surveys,
- emotional and psychiatric implications,
- the role of infectious agents,
- the study of the nature of inflammatory response, and
- clinical trials of new forms of therapy.
A partnership between physicians and researchers interested in the study of these diseases, along with patients, their families, and their friends, is the best hope toward finding the cause or causes, and the cure, of inflammatory bowel disease. Please support the GI Society’s educational and research initiatives.
Want to learn more about inflammatory bowel disease?
We have several related articles that may be helpful:
- Inflammatory Bowel Disease
- Crohn’s Disease
- Ulcerative Colitis
- Short Bowel Syndrome
- Biosimilars
- Survey Results: Biosimilars
- Biologic Coverage for IBD
- Therapeutic Drug Monitoring
- Medical Marijuana and IBD
- IBD and the Balanced Dinner Plate
- IBD & Pregnancy: Meeting the Challenge
- BadGut® Stories
- Living with IBD: Tips From Our Support Groups