
Is Your GI Condition Affecting Your Bone Health?
By Gwen Ellert, BScN, MEd, RN
Osteoporosis is a bone disease characterized by low bone density, and the deterioration of bone quality (strength), which can lead to increased risk of fracture. Bone loss happens slowly over several years. Still under recognized and under treated, bone fractures from osteoporosis are more common than heart attack, stroke, and breast cancer combined.
At least one in three women and one in five men will break a bone due to osteoporosis in their lifetime. The most common areas for bone loss are the forearm, spine, hip, upper arm, or shoulder. Bone health is not considered ‘urgent care’ and often not discussed at a doctor’s visit, even after you have suffered a broken bone. Osteoporosis Canada statistics sadly note 28% of women and 37% of men who suffer a hip fracture will die within one year.
GI Conditions Can Affect Bone Health
Several gastrointestinal conditions have been associated with low bone density and osteoporosis. Research shows bone fractures (broken bones) are almost 2 times as common in individuals with clinically diagnosed celiac disease as in those without the disease. In addition, the incidence of fracture among persons with inflammatory bowel disease is 1.4 times greater than that in the general population. Bariatric surgery patients have approximately 1.2 times increased risk for fracture.
More About Our Bones
Bone is living tissue that forms and resorbs all our life in a process called bone remodeling. Bone tissue must be developed and maintained through proper nutrition and bone strengthening activities from a young age. We build more bone than we remove until about age 16-20 for females and 20-25 for males, at which point we reach our maximum, or peak bone mass. Similar to managing our first bank account, we want to deposit as much money (bone) as possible for our future. We can only add to our ‘bone bank account’ until we reach our ‘peak bone mass’. Our bones stay stable until we are in our mid-thirties, after that point we must live on what we have deposited (formed), that is, the balance starts to shift, and we will remove more bone than we form or deposit.
Primary osteoporosis is bone loss due to genetics (DNA from parents), age, and/or post-menopause factors. Genetics can account for 60-80% of our bone loss. Age-related loss naturally starts at a rate of 0.5-1% a year, after a person reaches their mid-thirties; in other words, after their bones have reached their peak bone mass and stabilized. For women, rapid bone loss of 1.5-3% a year occurs for five or six years around menopause before gradually slowing to 1% loss per year.
For men, one in four over the age of 50 will suffer an osteoporosis-related fracture. Notably, hypogonadism, or low testosterone in men, is a risk factor for osteoporosis.
Immobility, disease, or medications are secondary causes of bone loss or osteoporosis. Diseases such as celiac disease and Crohn’s disease may result in malabsorption of calcium, vitamin D, and other nutrients, and medications such as prednisone and aromatase inhibitors (medication used in the treatment of breast cancer in postmenopausal women and for gynecomastia in men) can affect a person’s bone at any age. These situations present the need to take greater steps to achieve your highest peak bone mass and protect your bone health as you age.
A Quick Fracture Risk Assessment
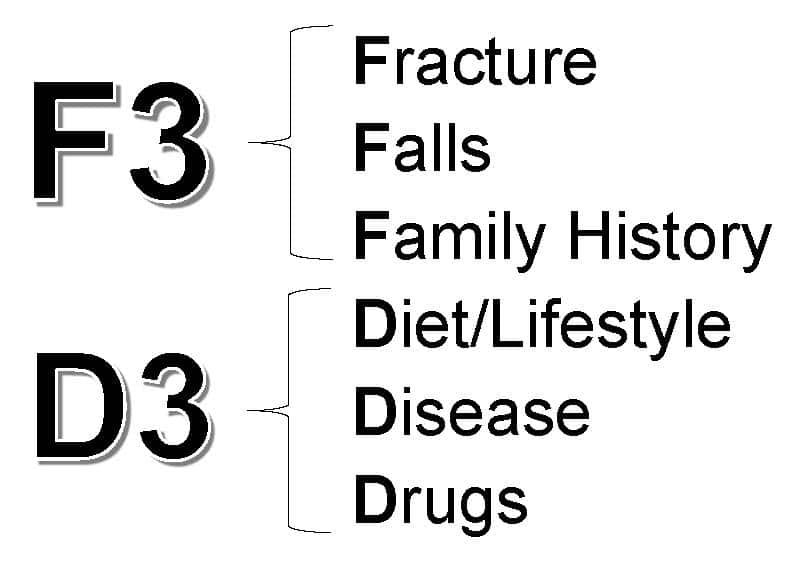
F3D3™ is a quick, bone health self-assessment tool. If you answer YES to any of the questions, discuss the question with your healthcare professional at your next visit.
Fracture
Have you lost height, 6cm /2.5” since tallest height or 2.5cm/ 1” in past 3 years? Height loss may signal a vertebral (spine) fracture.
Have you broken a bone, from a low-trauma injury, after 45 years of age?
Falls
Are you over age 65 and fallen more than once in the past year? More than one fall in previous 12 months increases the risk of fracture.
Family History
Did either of your parents have stooped posture or fracture a hip? Genetics may determine up to 80% of the risk for osteoporosis.
Diet/Lifestyle
Did you have less calcium and vitamin D than the recommended daily dietary and supplemental intake? Calcium daily total consumption (diet plus supplement) required for your age: 4-8yo 800mg; 9-19yo 1300mg; 20-50yo 1000 mg; 50+ 1200 mg
Did you have less sun exposure than 10-15 min/day, with no sunscreen, arms and legs exposed to the sun, and without taking the recommended vitamin D supplement? Vitamin D daily intake if under age 50, 600 IU- 1000 IU; if over age 50, 800 IU–2000 IU
Did you exercise less than the recommended 150 min/week of moderate exercise or 30 min/day five times a week? Exercise should include weight-bearing and resistance/strength training.
Do you smoke?
Did you drink more alcohol than the equivalent of two glasses of wine per day?
Disease
Do you have a disease that may cause bone loss, (e.g., Crohn’s disease or celiac disease, rheumatoid arthritis, alcoholism, liver disease, diabetes, anorexia nervosa)?
Have you had bariatric surgery?
Drugs
Do you take medication that may increase your risk of bone loss, (e.g., glucocorticoids (prednisone), medication to control thyroid hormone, or proton pump inhibitors (PPIs))?
Do you take a medication that might increase your risk of falling (e.g., sleeping pills, blood pressure medication or pain medication)?
Further Assessment
Along with your age, gender, and the questions such as those above, a clinical evaluation may include assessment of your bone density, bone quality (strength), and laboratory tests.
A bone mineral density (BMD) scan is a non-invasive procedure that measures the amount of bone material in a defined area of bone. BMD is most commonly done using a dual energy x-ray absorptiometry (DXA) machine. The results are reported as a T-score or a Z-score, depending on your age and gender.
A T-score is the number of standard deviations (SD) that your bone density is above or below what would be expected in the average person of the same gender at age 30. For each SD reduction in bone mineral density, your risk of fracture doubles. Your results will indicate if your bone density is: normal, low or you have osteoporosis.
For children, most pre-menopausal women, and men, a BMD-DXA scan will be reported as a Z-score. Z-scores cannot be compared to T-scores. A Z-score is matched to an average person your own age and is useful where enough data exists for comparison. A Z-score of -2.0 SD or lower is defined as below the expected range for age and above -2.0 SD is within the expected range for age.
FRAX™ measures bone quality without an invasive procedure and is the most common international, 10-year fracture risk assessment tool. It is most accurate when completed and explained by a professional aware of the nuances in each question.
Another measure is the Canadian Association of Radiologists and Osteoporosis Canada (CAROC) 10-year fracture risk assessment tool, with a database specific to the Canadian population. A BMD-DXA T-score for the femoral neck is required to complete the evaluation.
These tools can be used for patients who have not received any prescription osteoporosis therapies. Both are freely available online. FRAX™ will estimate your risk of a major osteoporotic fracture (in percent), CAROC is designed to predict whether you are at low risk, moderate risk, or high risk, of a fragility fracture in the next 10 years.
Finally, based upon your lifestyle choices and medical history, your doctor may use biochemical or laboratory tests to rule out secondary cause of bone loss such as calcium and vitamin D deficiency, parathyroid and thyroid involvement, or low levels of sex hormones.
Outlook
The good news is that, for many individuals, the process of bone loss can be slowed down or sometimes reversed by a few lifestyle changes, along with non-pharmaceutical and pharmaceutical therapies.
Research on persons with celiac disease shows that after maintaining a strict gluten-free diet for one year the bone loss can slow down. With inflammatory bowel disease, work with your specialist to promote adequate absorption of calcium, vitamin D, and other necessary nutrients to protect your bones. For those considering bariatric surgery, talk with your doctor about a bone health care plan to insure optimal nutritional intake and absorption. An appropriate exercise routine, which includes regular weight-bearing and resistance exercises, is necessary for everyone. If the appropriate diet, exercise, and lifestyle changes are not sufficient, there are several proven medication options to consider so you can maintain strong bones to carry you through the rest of your life.
The GI Society encourages and supports a discussion with your doctor about genetics, age-related risk factors, nutrition, exercise, and an appropriate bone health plan, especially for those at high risk of a future fracture.
Bone Health Basics Book
Osteoporosis is a major health and economic problem and is increasingly common with age in both men and women, and with some diseases and medications. For many people, the process of bone loss can be slowed down. Prevention and early treatment are essential. Bone Health Basics: Tips for Preventing and Managing Osteoporosis is an excellent resource with easy-to-understand information.
Discover methods for self-managing your bone health and preventing fractures. Become familiar with various treatment options for women and men who have osteoporosis. This book will help you to know what is going on inside your body so you can ask the right questions and get the information you need in order to make relevant and timely decisions about your own health. Available as ebook or paper copy through Friesen Press bookstore, Amazon, and Indigo.
Gwen Ellert, MEd, BScN, RN
A consultant and educator, Gwen authored and published the bestselling The Arthritis Exercise Book, accompanied by workshops and videos, aimed at helping people with arthritis live their lives to the maximum. Following the success of The Arthritis Exercise Book, she co-wrote two editions of The Osteoporosis Book with rheumatologist Dr. John Wade, which were endorsed by Osteoporosis Canada, and the third and fourth editions retitled The Osteoporosis Book: Bone Health with Dr. Wade and pharmacist Dr. Alan Low. It is currently being used in the American Bone Health Peer Educator Program. Her nursing and health promotion background, in conjunction with her personal experience managing her own rheumatoid arthritis, osteoporosis, and celiac disease, has made her a strong advocate for skeletal medical issues. Gwen co-founded a chapter of the Rheumatology Nurses Society and is in constant demand as a conference and workshop presenter. She is also on the Board of the Canadian Society of Intestinal Research.















